Green FHIR APIs,
Climb Mount Fuji,
Come see the sunlight!
*Variation on Kobayashi Issa “O, Snail”
 My second UGM (Epic’s User Group Meeting) offered a great perspective on the thousands of users on Epic coming together to share, exchange, learn, and advance their practices. Gathering around 13,000 attendees, Epic’s team has done a wonderful job just like a year before, making the atmosphere friendly while highly professional. The unique charm of Wisconsin, and Madison in particular, makes it a truly outstanding conference with a myriad of learning opportunities.
My second UGM (Epic’s User Group Meeting) offered a great perspective on the thousands of users on Epic coming together to share, exchange, learn, and advance their practices. Gathering around 13,000 attendees, Epic’s team has done a wonderful job just like a year before, making the atmosphere friendly while highly professional. The unique charm of Wisconsin, and Madison in particular, makes it a truly outstanding conference with a myriad of learning opportunities.
Going over my notes, comparing UGM2022 to UGM2023, I can clearly see a change. Aggressiveness of 2022 smoothed down and was transformed into, what it looks like, a new face of Epic – slowly but surely delivering on all the expectations and softly pushing forward.
I was curious to see what has changed over the last year and what was on the cards moving forward, so let’s go over my most notable impressions from UGM’23.
Denials, denials once again [Slicer-Dicer for improving RCM]
Denials have always been an issue in healthcare – a complicated, bleeding, never-healing wound on the body of revenue cycle departments everywhere. In the past few years, the volume of denials is unprecedented, and it’s only going up with more restrictive measures being taken around utilization management. Many providers feel they move one step forward and payers have already driven a mile. How does Epic keep up with constantly worsening denials issue? Slicer Dicer is their answer.
Talking to over 100 providers, I was quickly reminded that being on Epic is not the same as utilizing the software suite to its fullest given the variability in experiences and access to features that people were sharing. Slicer Dicer gives you a good analytical tool for denials, though I do not really see any true innovation here. The payer-provider platform would be a true breakthrough here when leveraged to the full extent, but not until we make our beloved payers finally start using FHIR APIs.
Slicer Dicer is a good tool in experienced hands, though it requires a great deal of customization. One of the biggest problems is categorizing denials properly by the root cause. I am a firm believer we need to develop a common industry-wide language on this matter so the technology can fully respond to RCM needs. Root-cause and categorization of denials has always been an issue, but recognition of the cause-specific patterns makes it actionable.
All the audits coming in as “medical necessity” denials are being labeled manually still, slipping through the cracks, delaying payments and, potentially costing your organization same is not the total denials amount. Lots of potential improvements and mapping could be done here to alleviate the manual burden of this process and speed up payments.
Payer-Provider Platform
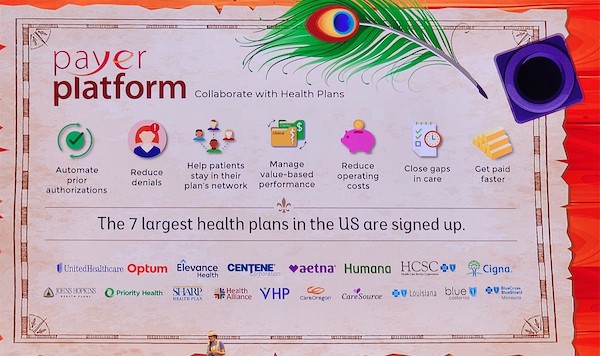 At UGM last year all we talked was Hospital at Home and Payer-Provider Platform. Well, it is all moving along. Mayo’s success with the platform was motivational to many during the presentation in 2022 and we do see the fruits of it in 2023. Providers are ready to share whatever data they are being asked for just to finally reduce the administrative burden and beautify their RCM suite. All the national payers are now on the platform.
At UGM last year all we talked was Hospital at Home and Payer-Provider Platform. Well, it is all moving along. Mayo’s success with the platform was motivational to many during the presentation in 2022 and we do see the fruits of it in 2023. Providers are ready to share whatever data they are being asked for just to finally reduce the administrative burden and beautify their RCM suite. All the national payers are now on the platform.
Tapestry is great, but the Platform will be that long-waited revolutionary tool just in few years from now if users keep on pushing for it. Epic is working day and night, but don’t expect too much yet. Without a doubt, the day will come when we will be able to happily wave goodbye to “no prior auth on file”, “denial CO50 for medical necessity”, along with many other time-consuming and labor-intensive issues I’ve personally had the pleasure of observing for the past 13 years.
VBC (C for complicated)
Value-Based Analytics in Epic continues to grow and deliver. It’s getting easier to monitor pay-for-performance contracts and move away from paper-thin margins. In addition to the usual – wellness visits, real-time workqueues, and medication adherence, we got some new features on the VBC performance management suite. Moving forward Epic will offer custom measures for state and payer-specific programs.
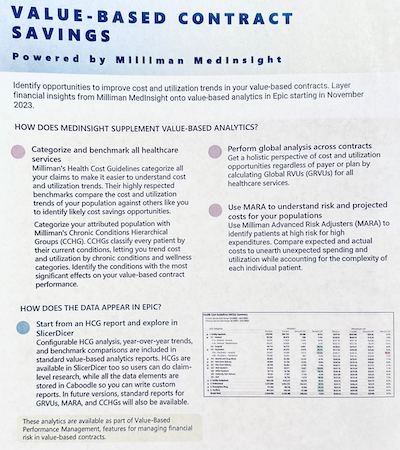 I was very pleased to find out about Epic-Milliman partnership. It was sealed almost a year ago and all the users of Epic value-based analytics will be able to access it in November of 2023. Calculating utilization costs even for line items is now at your service. Milliman is known in the market for their highly diverse data sets and will truly make a difference for those folks on VBC contracts. Though only 6 Milliman modules will be available through the partnership with Epic out of 18 developed so far, I was impressed with the functionality and simplicity of this tool when I saw their demo in the exhibit hall.
I was very pleased to find out about Epic-Milliman partnership. It was sealed almost a year ago and all the users of Epic value-based analytics will be able to access it in November of 2023. Calculating utilization costs even for line items is now at your service. Milliman is known in the market for their highly diverse data sets and will truly make a difference for those folks on VBC contracts. Though only 6 Milliman modules will be available through the partnership with Epic out of 18 developed so far, I was impressed with the functionality and simplicity of this tool when I saw their demo in the exhibit hall.
Another positive take: Payer-Identified Care Gaps for Outreach and Analytics. Payer-provider platform is now capable to do Care Gaps Exchange (you can also do it the old way through Data Ingestion and Normalization Engine). The downside is that the platform is actively growing, and you might not find all your major payers on it. But if you do, it’s a big win and could mean lots of extra money. Despite being a great tool, it creates some problems when it comes to gap closure execution. Given that providers are experiencing more pressure to engage their patients at the time of the visit, there should be a lighter plug-in patient engagement tool available.
Provider Directories
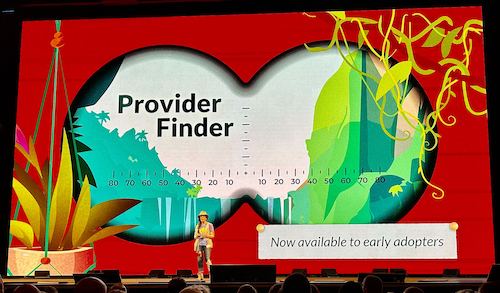
Provider directories have been a mess for the longest time. Several companies are working on solving this puzzle and Epic is actively working in this direction too.
I revisited provider directories a year ago to sadly find no big improvement. Providers’ locations, availability, particular areas of expertise, languages spoken were scattered all over the place between payers, provider organizations, and scheduling platforms. Very curious to see what Epic will come up with now that this is available to early adopters.
One more step towards shoppable healthcare.
Enhanced Efficiency: The Trio of Haiku, Canto, and Rover
Epic is aware of the “In Basket” issue for providers and is actively trying to solve it. Last year I had numerous conversations with docs being overwhelmed with the number of messages they received during one shift; in some cases, it could reach over 400 messages. With a rapid growth of remote care, there was a clear need for compact easy-routing solutions and alternative ways of provider-to-provider and provider-to-patient communications. It seems like now they are truly building momentum.
Haiku and Canto, in addition to Rover, makes a great trio to help manage physician overload, to enable providers to do their work efficiently in any environment, and to serve their patients best. Fully developed on iOS and Android it makes a powerful bundle pushing the limits of traditional care settings.
Conclusions
UGM’23 showcased Epic’s transformative journey, marked by a measured evolution and steadfast commitment to enhancing healthcare practices. As the industry continues to evolve, Epic’s innovations and partnerships hold the promise of a more streamlined and patient-centric future. As always, Epic has a lot to catch up on. There is a huge demand for lighter population outreach tools, for easier collections functionality, for fully automated authorizations. Nevertheless, Epic has always given hope and the tools to providers to make healthcare better.
Thank you note
I am profoundly grateful to the Epic team for this wonderful opportunity to learn, meet great people, enjoy beautiful Wisconsin. Please, keep on pushing!




0 Comments
Trackbacks/Pingbacks