Insights from the Providence journey to value based care delivery
“Providence on average serves about 5.2 million unique patients every year across all our markets, from Alaska all the way to Northwestern Texas. The population that is under some level of financial risk exposure under the HCP LAN (Health Connect Partner Learning Action Network) between categories two and four are about 1.7 million of those 5.2 million, and this didn’t happen overnight. Of those 1.7 million, about three quarters (~1.3M) of those are in categories three and four, where we either have shared or full financial risk in those populations.”
Key Takeaways:
- PNW-based Providence is a large, multi-hospital system that has become a notable leader in the transition to value based care over the last decade.
- Equitable whole-person care requires flexible resource allocation and a shift from enterprise-centric to network-based (or “portfolio of services”) care models
- Cloud tech and real-time data synthesis across settings enable agile, proactive population health management at scale
- Redefining ROI around long-term patient outcomes and health equity is critical for sustainable value-based transformation
Listen to the podcast by using the embedded player below, or on your favorite podcasting app via this link.
Transitioning from diagnosis-centric to whole-person care
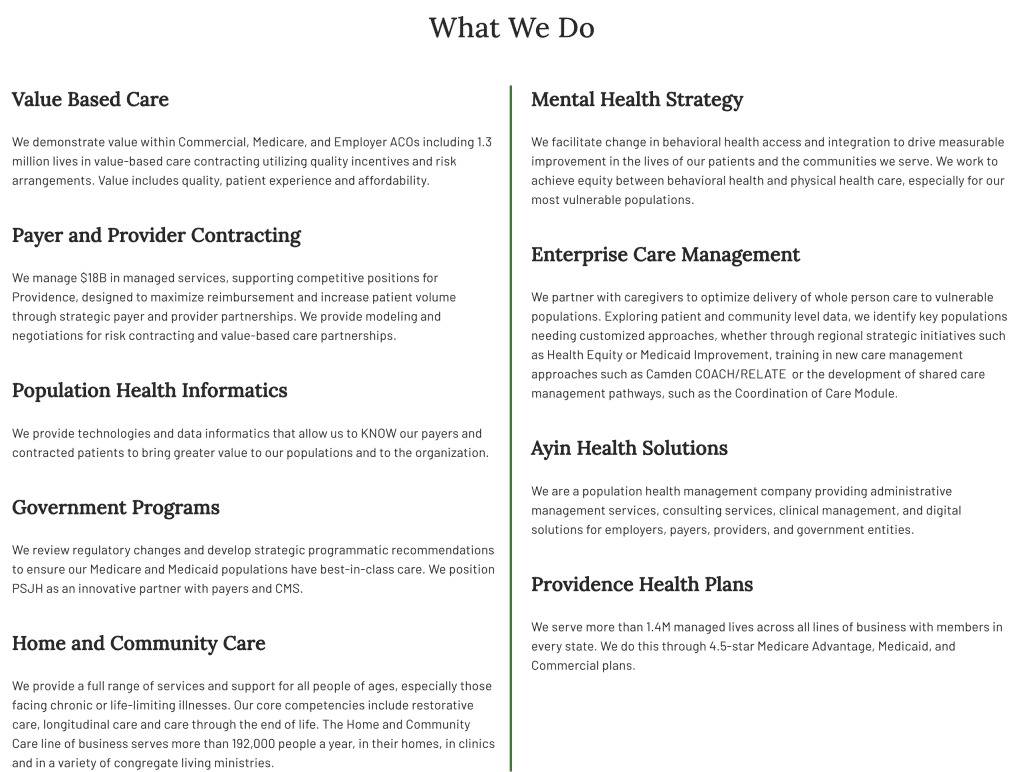
In this Chilcast episode, John Moore sits down with Deepak Sadagopan, COO of Population Health at Providence and CEO of the Providence Medicare ACO, Health Connect Partners, to discuss strategic best practices for healthcare executives navigating the transition to value-based care (VBC).
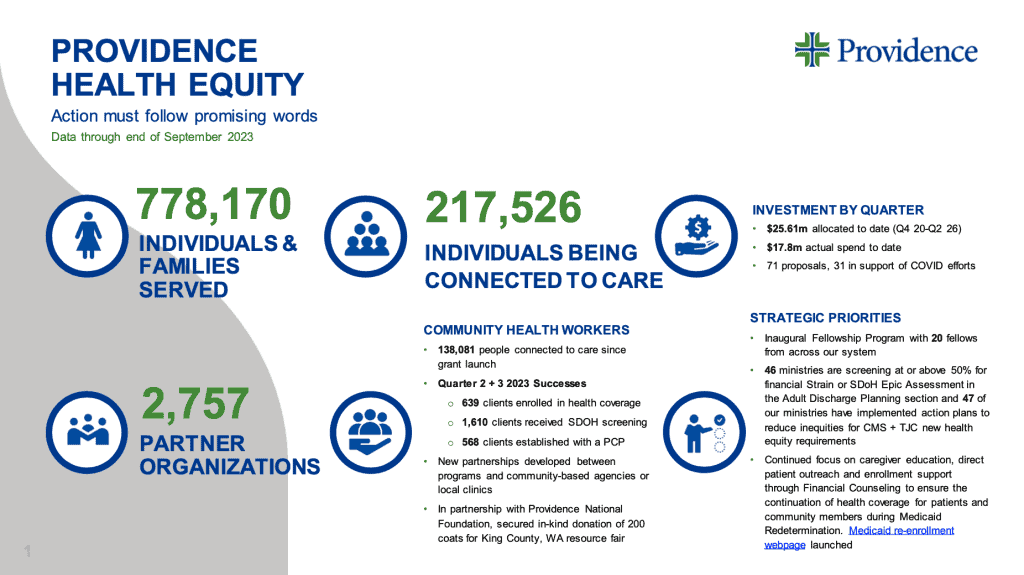
Deepak emphasizes that achieving equitable, whole-person care requires a fundamental shift from enterprise-centric models to network-based risk sharing. As care delivery becomes increasingly distributed, success in VBC hinges on flexibly allocating resources based on an accurate understanding of specific population needs rather than equal distribution of services for everyone. Providence’s targeted investments in community health workers and education to address maternal mortality and hypertension disparities exemplify this approach, yielding significant improvements in equity without substantial additional financial outlays.
The Cloud is an enabling technology
Cloud technologies emerge as a critical enabler of agile, proactive population health management at scale. Deepak highlights how cloud-based data models allow organizations to efficiently synthesize information from multiple sources and settings, applying real-time intelligence at the edges. This marks a significant advancement from the previous era of siloed, on-premise data, empowering healthcare organizations to rapidly identify risks, close care gaps, and drive better outcomes across diverse populations.
Redefining ROI for modern care models
Crucially, Deepak argues for redefining ROI around long-term patient outcomes and health equity as a strategic imperative for sustainable VBC transformation. While core systems like EHRs continue to be evaluated based on productivity and efficiency gains, population health investments should be assessed on their ability to improve care quality, patient experience, and equitable access. Deepak notes that initiatives aimed at health equity may not yield immediate financial returns but are essential for reducing total cost of care and optimizing resource utilization over time.
Actionable takeaways aplenty
Throughout the discussion, Deepak returns to the centrality of the patient perspective in guiding any VBC strategy. By elevating patient-reported outcomes as a key accountability metric and redesigning care delivery around patient priorities like recovery time and care proximity, healthcare organizations can align their investments and operations with the ultimate goal of delivering value to the populations they serve.
For healthcare executives steering their organizations through the VBC landscape, Deepak’s insights provide a roadmap for success: embrace flexible, network-based risk models, harness cloud technologies for agile population health management, and anchor ROI in long-term patient outcomes and health equity. By adopting this strategic framework, leaders can position their organizations to thrive in the era of value-based care.
5 Notable Quotes
- “If you think about [risk-based contracts] in terms of the networks of care that I described earlier, the value based care ecosystem is really heading towards networks where financial risk is not concentrated in one organization alone, instead it’s concentrated in a network of care delivery and that network shares the financial risk. And then every organization needs to ask itself: what role are we playing in that network? Are we a participant in that network, in which case are we taking a portion of the financial risk that is appropriate to the scope of care that we deliver? Or, are we taking the risk – do we have the bandwidth and the ability to build the network and actually create the overall infrastructure to actually support it?” (21:16)
- “We’ve been able to make [equity-centric] changes as a result of focused investment in community health workers, with education and by creating awareness in primary care settings about specific needs for these populations. We’ve been able to move the needle a little further ahead, demonstrating that it doesn’t take too much additional financial resource to support achieving equity: It takes intent, purpose and it takes the ability to be flexible in how you resource the delivery of care, recognizing that the need for care delivery resources are not equal across all populations.” (25:58)
- “Value-based care has an important role to play in the economic sustainability of healthcare delivery going forward. I wouldn’t say VBC is going to completely replace the existing economic model – I think they will continue to operate side by side for the foreseeable future. I do think the availability of cloud technologies and the ability to quickly create and operate data models at scale across enterprises has made it easier to align information infrastructure in a value-based care world.” (33:02)
- “You cannot speak of value without talking about what it means from the perspective of a patient? What does it mean from the perspective of a provider? What does it mean from the perspective of a payer? Of all of these perspectives of what value means in healthcare, the ones that actually takes precedence and impacts you and I and every other individual is the perspective of the patient. When you ask the question to an average consumer who’s unaware of all of these models, in its simplest terms, it comes down to what’s the quality of life that I lead and what’s the quality of life that my family leads?” (34:47)
- “The way we look at ROI for our core care delivery (eg EHR, RCM) systems, it’s really about does it improve the productivity of our caregiving staff? Does it make [delivering care] easier? Does it drive efficiency in our administrative operations? When you look beyond that – like in a population health setting – we look at returns in value-based care. Is the technology promoting our ability to close care gaps faster? Are we driving better outcomes? Are we able to identify a greater proportion of chronic conditions in our population so that we’re able to align care resources to that? The way you evaluate ROI really depends on the purposes that they serve and who’s gaining value from that.” (42:55)




Thank you for sharing! How did having Master Data Management services help propel the solution(s) for your organization? In the Patient/Member matching?
Hi there! To clarify, I have a masters in healthcare delivery and economics. I am not sure I understand the question pertaining to patient matching..