COVID-19 is alive and well in the U.S. In the last six days alone, COVID cases have increased by over 386,000. We never got over the first wave and here we go again with a dramatic rise in new cases in the majority of states across the country.

The previous surge, targeting the mid-Atlantic, Northeast states and west coast, had a dramatic impact across the country as a national healthcare emergency was declared and elective procedures were put on hold. Patients also began avoiding the emergency room and cancelling visits to their doctor for fear of contracting COVID-19. We never really got over the first wave with the pandemic laying bare many ills of the U.S.’s current healthcare system in spite of the heroic efforts of healthcare workers. This is likely only to get worse in foreseeable future.
COVID-19 + Fee for Service = Bad Marriage
What may turn out to be one of the biggest ills in healthcare is the current form of reimbursement. The predominant model, fee-for-service (FFS), only pays out when services are rendered. During this pandemic most healthcare services have been put on hold and thus no payment to providers. This has put tremendous economic strain on healthcare providers of all sizes, leading to significant cost controls including laying off or furloughing staff, cutting pay and benefits and in extreme cases, some smaller provider practices have simply closed.
Over the last decade or so, there has been an ever so slow migration towards a new payment model, value-based care (VBC). Under VBC, a provider organization delivers care but instead of a flat FFS rate, they are paid based on quality (Q) and cost ($) of care: Value = Q/C In a true VBC scenario, the provider takes on the associated risks of managing a given population’s/patient’s health in return for potentially higher reimbursement.
Despite the potential upside of VBC, migration to this new reimbursement model has been painfully slow. A big part of the problem has been the need for healthcare providers to completely reinvent themselves and how they operate to capitalize upon VBC wherein they may be paid on a per patient per month model for all care rather than for specific services.
Telehealth Surge, Yesterday’s News – There is Something Bigger at Play
There has been a tremendous amount of hype regarding the dramatic rise in telehealth visits as a result of COVID-19 – most pundits stating that the pandemic has accelerated telehealth adoption by at least a decade. Fine, all well and good but I think this is a relatively shallow view of how COVID-19 will impact the industry. The pandemic’s biggest impact will be to accelerate the adoption VBC reimbursement models for one simple reason – economics.
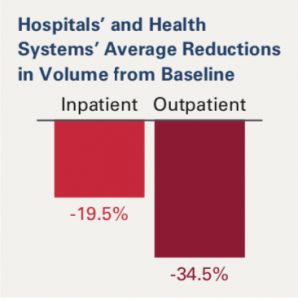
According to the American Hospital Association’s latest report, providers are expected to lose over $320B in 2020 due to COVID-19. As provider compensation today is based largely on volume in a FFS world, the significant decrease in elective procedures and patient visits has had real economic consequences.
However, what if those healthcare organizations had a significant proportion of their compensation based on a VBC model wherein they would be paid not on the volume of visits and procedures they performed but on how well they managed a given populations’ health over some contract based time period being paid on a per member per month (PMPM model)? As long as the provider met certain quality and cost containment guidelines, might they be better off than they are right now?
My guess is yes, with some caveats.
- That the provider is committed to making the transition to VBC as it is challenging on multiple fronts to accomplish – it’s as much cultural as it is technological.
- The payer(s) are willing to provide fair compensation and timely delivery of needed datasets (claims data, care gaps, referral patterns, etc.) to facilitate care.
- Reporting requirements are fair, not onerous with each organization (payer and provider) committing to working towards same overarching goal.
And while everyone in this sector seems to scream: “disrupt this, disrupt that”, “the pandemic will forever change healthcare”, “lead by innovation”, I am a bit more pragmatic in stating simply: Follow the Money.
If we can change the incentive structure that currently exists in healthcare that supports the status quo, we can foster disruption, we will see major advances in innovation and the bump-up in virtual care we recently saw will be sustained as provider organizations seek new ways to manage their patients’ health in cost effective ways without diminishing quality of care or quality of life for their patients.
BCBS-NC Jumps the Shark
On June 24th North Carolina’s second largest payer announced a very progressive, if not aggressive program to prompt independent physician practices to migrate to a VBC/ACO model. While many a payer has put forth a VBC program of one flavor or another, with most focusing on Medicare Advantage, the BCBS-NC is arguably the most progressive program to date and bears close watching.
For BCBS-NC the objective is clear, keep independent practices in business as well as independent as such ambulatory practices are known for being an effective foil to large health systems to control costs. For independent practices, they get a much needed lifeline of economic support at a time when their financials are severely stressed.
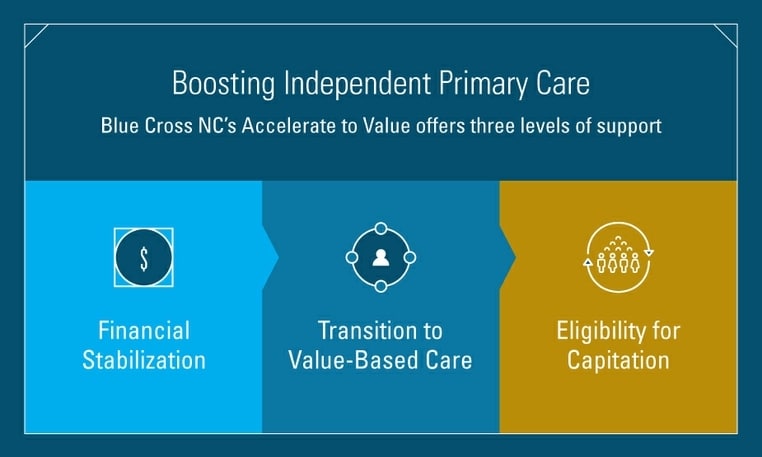
The plan is broken down into three levels:
- Level One: Financial stabilization wherein BCBS-NC will pay providers who demonstrate they have BCBS-NC members by comparing visit rates in 2019 to 2020 and true-up payment for all of 2020 and carry forward into 2021. Two nice bones BCBS-NC throws into Level One are they will not claw-back payments if BCBS-NC overestimate what a practice is due nor are there any additional reporting requirements. The only requirements that BCBS-NC asks for are for the practice to remain open, delivering care to its members via care coordination, visits (virtual and in-person, etc.).
- Level Two: In accepting financial stabilization, practices contractually agree to join the Blue Premier ACO program by Jan. 1, 2021. BCBS-NC has partnered with Aledade to assist providers with on-boarding to the Blue Premier ACO. (This could be a big win for Aledade!)
- Level Three: In 2022, practices will become eligible to move to a fully capitated model of reimbursement with fixed monthly payments for meeting the healthcare needs of the BCBS-NC member population in their care.
Devil is in the Details
With this announcement, BCBS-NC has clearly taken a big leap (jumping that shark) to aggressively migrate independent practices to a VBC model. How it will be received by these providers remains to be seen and there are risks for both BCBS-NC and the practices that sign on to this program. Some that readily come to mind are:
- How will BCBS-NC ensure that the practices that sign-up for this program clearly intend to stay in practice for several years? BCBS-NC is making a pretty substantial investment that will take a few years to recoup.
- [A corollary to above] How will BCBS-NC ensure it is recruiting practices into this program that have a good history of delivering quality care? Is there a screening process by which BCBS-NC will accept or deny a practice from joining?
- How trusted is the relationship today between practices and BCBS-NC today? Is it greater than the trust between these practices and the large healthcare systems in their region, or that of a P.E. firm that just offered a lucrative deal to buy their practice?
- Just how robust is the Blue Premier ACO that BCBS-NC announced in Jan. 2019? I know it is still early to measure success of an ACO a year and a half later, but I do wonder what their success has been in recruiting practices to this ACO. Maybe this latest move was an attempt to drive adoption, which may have been lackluster, especially in this age of the pandemic.
All Good
Regardless of those caveats, I’ll be the first to say that I really do like what the leadership at BCBS-NC has put together. It is a nice balance of pragmatism, needed financial assistance to independent practices and what seems to be a good glidepath to VBC for these practices. I want to see this program succeed and modeled elsewhere in the country for in the end, it will be programs such as these that will truly disrupt healthcare for the good of all.




0 Comments