While there is no single complete definition of ‘primary care’ in the United States, most of the various definitions agree that primary care is first contact care covering a broad list of diagnosis, treatment, and professional roles. It’s focused on an individual relationship between a patient and a provider, where the provider plays a central role in the definition and distribution of care. Historically, the primary care provider (PCP) acts as a central organizer, “helping the patient define the conditions under which entry to professional services and continuation in care are appropriate.” Where other specialties see the patient only as needed, the primary care provider has an ongoing relationship with them.
Key Takeaways
- There are not enough hours in the day for all the clinical, administrative, and monitoring roles PCPs are expected to fill.
- Outside of new tools and options for engaging in direct clinical care, tools also exist to relieve other workflow and task burdens.
- For post-acute and post-discharge patients, an improved discharge process and better home monitoring offer both improved patient outcomes and give their primary care provider important visibility into their health status.
Unreasonable Expectations
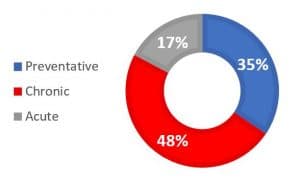
Figure 1: Use of Provider Time in Primary Care (U.S.) (Altshuler, Margolius, Bodenheimer, & Grumbach, 2012)
Increasingly, PCPs are acting more as a broad service provider. As systems condense more professional services and specialties or access to them becomes more constricted, PCPs find themselves forced into filling unfamiliar and clinically difficult roles. PCPs spend most of their time in chronic care management and preventative care, accounting for more than 80% of clinical hours. They report that they do not have enough time to provide what they consider to be adequate care for patient panels. Minimum adequate patient care in the three major categories (chronic care management, preventative care, and acute care) is estimated to require just over two hours per patient per year. Based on that standard, a panel of two thousand patients would require 11.3 hours of active clinical time for every day of the year, or 15.8 hours per day for a work year that provides for weekends and holidays.
In the upcoming Primary Care for the 21st Century Market Scan Report, we look at software, technologies, and platforms addressing these and other issues in primary care. Some tools are focused on direct care and access, or what we call the “front door to care.” However, there are many administrative, communication, and patient engagement solutions that are not involved with the patient’s first touchpoint with the healthcare system, but still offer significant value. Care coordination, transfer of care, and post-acute follow-up all cost time, effort, and resources for providers and staff. Relieving those administrative burdens allows more clinical time, and greater time spent working at the top of license.
Transition of Care Platforms
Care management platforms targeted at post-acute discharge placement and planning, like the one provided by CarePort Health, aim their solutions at each element of the transition from in-patient to out-patient care. The goal is an improved patient experience, ensuring that patients are going to locations with the right capacity and capabilities for their post-acute needs, while patients, providers, and facilities are all tied into the same communication loop. These products assist in discharge management, ADT tracking and management, and help to manage the complex process of referral, approval, and intake tied into the transfer of care process.
As patients transition between care facilities, it is easy to lose visibility into their health status, treatment progress, and emerging risks. Care teams most commonly resolve those gaps through phone calls or in-person communication and track them manually. By automating data sharing on cross-system patients, transition platforms can save significant staff time. By integrating that data into existing patient records and care management platforms, patient care is improved and potential gaps or risks are mitigated. As that data comes in, it can become part of the analytic record, allowing improved tracking and insight into important metrics. Visibility into patient activity at the post-acute facility combined with a better understanding of their care path reduces the amount of time needed for primary care providers to track their patients, to understand their care needs, and to ensure that they can get the time and care needed to avoid a readmission.
Post-Acute Remote Patient Management

Post-acute remote management platforms from teams like Current Health and Orion Health combine elements of remote monitoring with patient engagement, patient-reported outcome measures, and shared decision-making. At scheduled intervals throughout the day, or as needed, users access the platform through their phone, tablet, or over the web. Patients can be sent reminders for medication or other regimen adherence, the platform can launch queries to monitor vital signs or well-being, and providers can track other aspects of daily life that are relevant to a patient’s diagnosis. These platforms support the growing ecosystem of at-home medical equipment, allowing for vitals monitoring like weight, blood oxygen, blood pressure, or glucose. Some integrate conversational chatbots for symptom discussion or to provide feedback while engaging users in education and health monitoring activity. Meanwhile, the health system working with the patient receives data and responses as part of the care feedback loop.
PCPs can find significant value in better home visibility for these high-risk groups. They will not replace the standard post-discharge appointment, but these platforms give providers important additional insight into patient activity and more ways to monitor and engage patients in the most important parts of their post-discharge period. Equally importantly, as more data comes in and patients provide their own reactions to medication, testing, or other health activities, providers and care managers can modify those regimens in a much shorter timeframe than is currently allowable. Patients can also be actively involved in their health maintenance instead of just passively performing assigned activities, which has been shown to promote communication, improve adherence, and improve outcomes.
Conclusion
In addition to their traditional front door to care role, primary care offices monitor and engage with patients throughout their medical journeys, and these additional workloads take significant time and resources away from their overburdened clinical time. Tools like these can offer workflow and administrative relief to PCPs and their staff, easing their burdens while addressing important areas of patient care and promoting the best possible patient outcomes.




0 Comments