When legislation collides, and a call for the healthcare innovation equivalent to GAAP
Summary
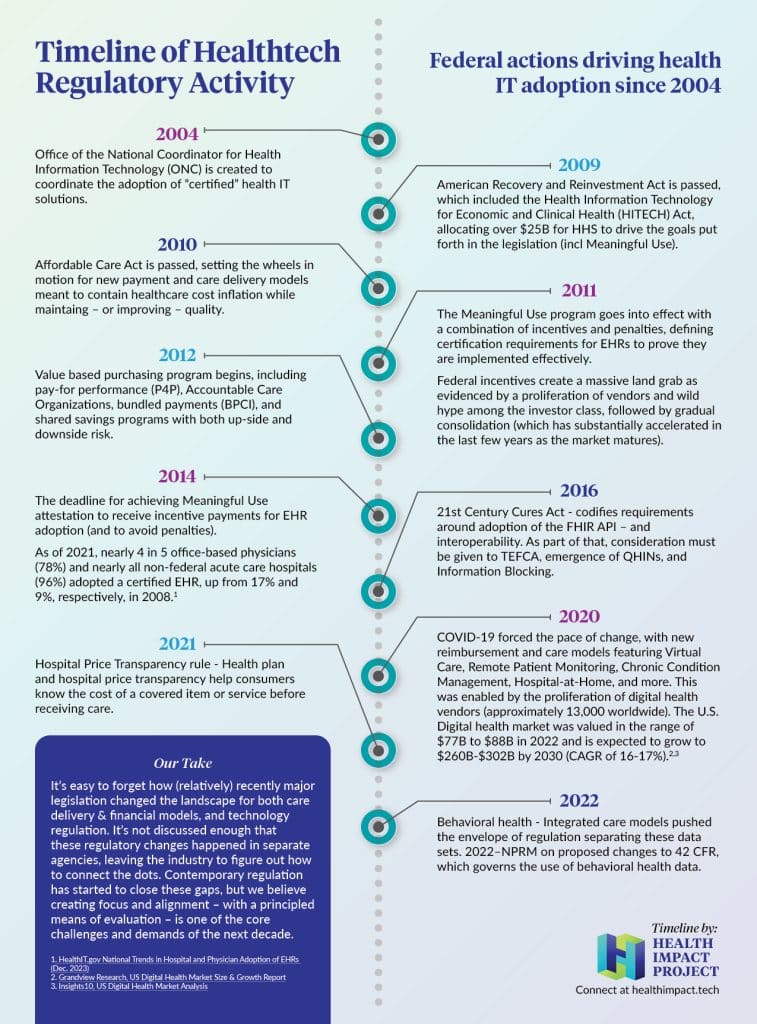
The conversation captured on this episode, as well as the next group one, both tie into our recently published article, “When world’s collide: How two decades of regulation both advanced and hindered our transformative vision of healthcare innovation.”
Takeaways
- Legislation has played a significant role in shaping the adoption of IT in the healthcare industry, but has come up against care model reform legislation that often doesn’t neatly align with IT maturity. This has created extra burden on decision makers who must balance these prerogatives.
- Challenges remain in assessing the value of technology, especially due to the complexity of current shifts in the economics of care.
- Our industry needs to develop its own equivalent of generally accepted accounting principles (GAAP) for evaluating the impact and return on investment (ROI) of health technologies. This is complicated by the moral mandate of the healthcare industry, where the outcomes of “free market forces” are not always best for the population being served. Any calculation of ROI needs to account for this double bottom line.
- Collaboration and a shared understanding of value are essential for driving industry success with technology use cases, which in turn should improve outcomes and experiences.
Listen to the podcast by using the embedded player below, or on your favorite podcasting app via this link.
Notable Quotes:
- Marie (5:10): “Value-based payment happened right around the same time as meaningful use. At the same time as we were making electronic health data available and incentivizing that, you’re also building new care delivery models. I think that’s critically important because when we talk about a concept like ROI, we expect those things to come together. But when we think about the origin of where we are right now, we didn’t always design together because we were figuring out what those things were at the same time.”
- John (11:46): “Healthcare is so political in the way that it’s reimbursed, the way it’s regulated. It’s constantly shifting, complicating the ability to assess ROI. Value-based care has completely different ROI than fee-for-service models when evaluating a technology…We’re dealing with many different economic systems, making it complicated for the board and executives in the C-suite to define what their objectives need to be to come up with something consistent for measuring and evaluating impact.”
- Marie (14:07): “We’re at a point where we’ve done so many different experiments over the last 15 years that we all have different languages even within healthcare, right? Everybody has different expectations of what the technology might do, whether you’re in the financial part of the business, the clinical part of the business, or some other part of the business. But ultimately at the end of the day, if you all can’t talk together, then you’re not gonna be able to sort of figure out whether that technology has been successful.”
- Curtis (18:47): “Ethical principles are so important in medicine and healthcare. We have a structured way of how we do drug discovery and clinical trials; [p]rinciples around human subjects research. So what’s the appropriate level of rigor if we want to make an operational change to the healthcare system? If we’re going to introduce a new technology that is not clinical but we expect it is going to have clinical impact, what is that rigor? What’s the evidence we need before we’re comfortable rolling it out within a healthcare system? What are the guardrails to protect patients and make sure that we are not harming them as we learn?”
- Susan (21:14): “One of the difficulties in ROI is that we have to say, ‘Did that technology cause the improvement, or was it something else, or is it a number of factors?’ And then you have to tease out what contributed what to the [outcome] that you’re experiencing. Sometimes we simply can’t measure pre and post. You may come up with a great KPI to say something is improving, but we can’t go back in the past and say, what’s the baseline? What were things like before we actually implemented this technology?”




0 Comments