To this end, we are conducting a 10-minute web survey on clinician’s experiences using HIEs for care coordination. We want to understand how clinicians are using HIEs today in their daly activities. If you are a credentialed clinician with any experience using an HIE of any kind, we invite you to take the survey by clicking on this link.
In appreciation for completing the survey, we will provide a $50.00 Amazon gift certificate for the first 50 completed surveys we receive from verifiable clinicians (i.e. a working email address at the end of the survey). We are particularly looking for clinicians working in large group practices or in post-acute care but any care venue is appropriate. Just remember, you must be a credentialed clinician, have a good sense of how your HCO is or should be using an HIE, complete the entire survey and provide us with an email address to qualify (and also so we know where to send that Amazon GC). Don’t worry, we promise to never to disclose your name or the name of your organization and your contact details to anyone, for any reason.
Why are we doing this?
Simple. The days of thinking about HIE as basic plumbing are over. Enabling HIE remains complex and expensive due to the lack of interoperability across the heterogeneous EHR landscape found in most communities. At a recent conference, David Kibbe of DirectTrust gave a presentation with the following data points.
In one Arizona County there are…
Specific Data Points
Unspecific Data Points
|
While we certainly recognize why many still speak of HIE in the context of just stitching together communities of practice and their disparate EHRs; to truly move forward, healthcare leaders need to stop thinking that they are enabling HIE. Thinking within the construct of HIE is a natural, self-limiting proposition that does not focus on value realization.
Follow the Money – Network Management Critical
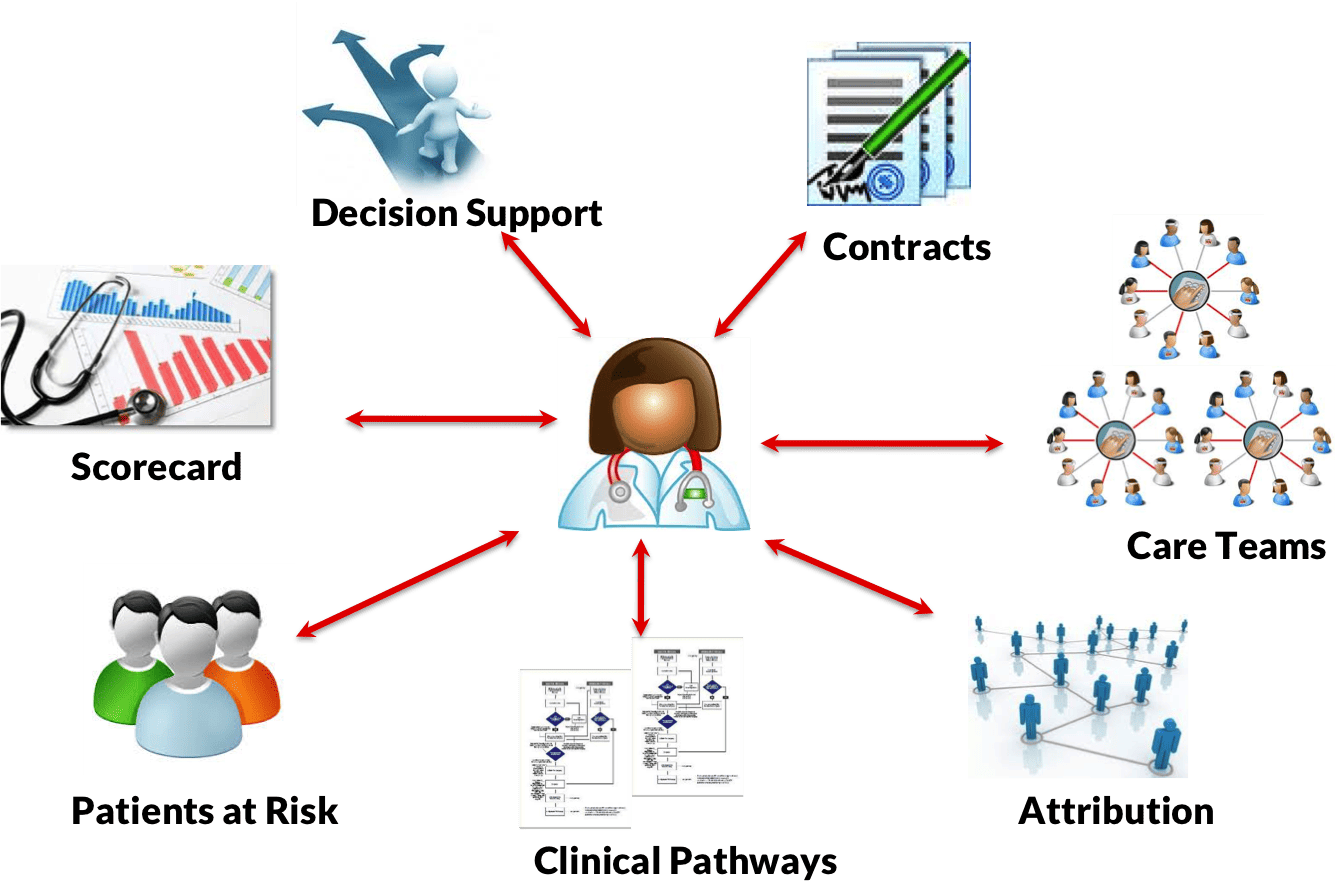
As the industry makes the massive transition from fee-for-service to value-based reimbursement models, the long-term success (or ultimate failure) of a healthcare organization will be highly dependent on their ability to effectively manage their clinician network, both owned and affiliated. And when we say manage, we are not talking about heavy-handed management, but more about ensuring that all in-network clinicians are aligned along the same goals and objectives to maximize reimbursement. Network of clinicians need to work together to accomplish such goals as:
- Successful care transitions that minimize readmits
- Managing care gaps
- Define, distribute and track clinical pathways
- Keeping those at risk of chronic disease from contracting the disease
- Effectively manage patients with chronic disease(s)
- Practice score-carding to identify outliers and take corrective action
- Assign attribution based on contract terms and clinician involvement
Virtually all ambulatory practices do not have the resources to address the above and their EHRs certainly won’t get them there either. Only the parent HCO has the resources and expertise to enable this advance functionality and it is their job to insure such is distributed to their network and owned and affiliated physicians.
Our hypothesis is that large HCOs are searching for ways to influence clinical processes and workflow outside their walls and will leverage their HIE infrastructure to do so. At the same time, community-based clinicians need better access to better information so they know what is expected of them when treating shared risk patients. In the next year, we will be looking at the ways that HCOs are building alignment within their networks of physicians – owned or affiliated – to establish common care goals and objectives that also maximize contract opportunities for everyone.
This survey is the first step in our research on the necessary transition from HIE to Clinician Network Management (CNM). Time to roil the industry and think beyond the limited confines of HIE to the value that can be delivered within a clinician network.




0 Comments
Trackbacks/Pingbacks