Several factors contribute to provider PHRs succeeding where others struggle:
Trust: Consumers trust their physicians more than employers and payers to look out for the best interests. If a provider suggests to a consumer that using their PHR would be advantageous, the consumer will take the suggestion more seriously and with less fear that data within the PHR will be used against them (denial of coverage, stigmatized, etc.) at some future point in time.
Value: Most of the better provider sponsored PHRs provide transactional tools that facilitate a consumer’s interaction with their provider including appointment scheduling, eConsults, viewing lab results and Rx refill requests. Independent PHRs or those sponsored by employers or payers simply do not have transaction capabilities with provider networks, end of story.
Data: While there has been some recent publicity on bad data that may exist in even a provider sponsored PHR, by and large the data therein is better and certainly more useful than what you’ll find in an employer or payer sponsored PHR, which is almost solely claims and PBM data.
But provider PHRs also have their fair share of challenges and shortcomings:
Tethered: Virtually all provider PHRs, for that matter virtually any sponsored PHR that a consumer may use is tethered to the sponsor and th consumer can not readily take records with them should they change plans/providers/location, etc. This is slowly beginning to change as leading providers such as Beth Israel Deaconess, Cleveland Clinic, KP and New York Presbyterian allow their customers to export their records to one of the Health Clouds (Google Health or HealthVault), but we still have a very, very long ways to go.
Siloed: Provider sponsored PHRs give only one facet of a consumer’s record, those notes, labs, meds, etc. that were provided through that specific provider/network. If the consumer has a several providers, both in and outside a given network, the consumer may well end up with more than one provider PHR but no aggregate PHR, unless of course they get all their records up into a Health Cloud.
Poor User Interface: Chilmark Research has seen many a provider sponsored PHR and by and large, they could use some good User Interface (UI) engineering, some nasty stuff out there. This may simply be an end result of the lack of attention paid to this aspect of the services a provider offers its community. Another reason may be the clinician perspective that most provider sponsored PHRs pursue, rather than considering consumer needs first.
Lack of Control: Yes, consumers trust their providers more than just about anyone else, but increasingly, consumers want more direct control of information (records) that is theirs. No, this does not mean that they can edit clinician notes, but it does give the option to choose who to share their records with, e.g., does a dermatologist need to know about an STD in college, 20 years prior?
As was discussed yesterday, Chilmark Research is seeing an uptick in provider interest to deploy and use PHRs that go beyond marketing and customer service. But to be successful long-term, providers must look at their PHR strategy more broadly and more inclusive of the full spectrum of the consumers’ needs, which will more than likely extend beyond the confines of what the provider can offer in their PHR deployment.
What New York Presbyterian (NYP) is doing with HealthVault is a good example. NYP wants to reduce re-admissions of cardiac patients upon discharge but fully realizes (as most hospitals have experienced) once a patient is discharged, they basically fall into a black hole and the hospital has little idea or means to track how the patient is doing in the ambulatory setting. By providing the patient with a portable, HealthVault account within the context of MyNYP.org, the patient is able to share their discharge notes with their primary care physician (PCP) and likewise, the PCP can upload progress reports to the account as well. This is taking care beyond the confines of NYP and its network, by putting the consumer in control, something that is rarely done today.
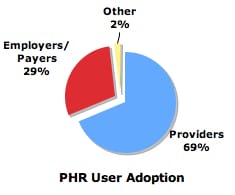
To some extent, the arguments put forth by Drs. Tang and Lee a month ago in the New England Journal of Medicine are true: Provider sponsored PHRs will be the true successors in the PHR market. But if providers continue their practices of keeping data siloed, tethered, in their control and offer a poor user experience, provider PHRs will be but a small step along the path to consumer-centric, consumer-controlled personal health record management. Now the million dollar question is: Is the consumer ready to take on this responsibility?




To your question, I would say that not all consumers are ready to take on this responsibility. I would say that those who are specifically experiencing a chronic condition–or those who have relatives for whose medical conditions they are entrusted–will. This may be the difficult part of this. EMRs have shown to speed treatment. PHRs have shown to enhance the doctor/patient dialogue and improve outcomes. Will everyone take this on? It’s hard to say. Those who can and have a vested interest will. My concern is for those patients who do not have regular access to a computer. Who will be looking out for them?
PHRs without link to an EMR are like using Quicken without access to a bank. What’s the point?
On a different note, design and user interface are huge factors in establishing trust in a product. In the early days of ecommerce, studies showed a 70% correlation between the quality of design on a site and users’ trust in the site.
I can’t fathom it being any different for PHRs. Interestingly enough, the builders of the PHRs are passing on the responsibility of design and UI to the providers that license them.