13 predictions about what to expect in digital health and health IT We can all agree that 2023 has...
From Silos to Synergy
The need for interoperability across systems is higher than ever. How can HCOs utilize APIs to create a better healthcare experience?
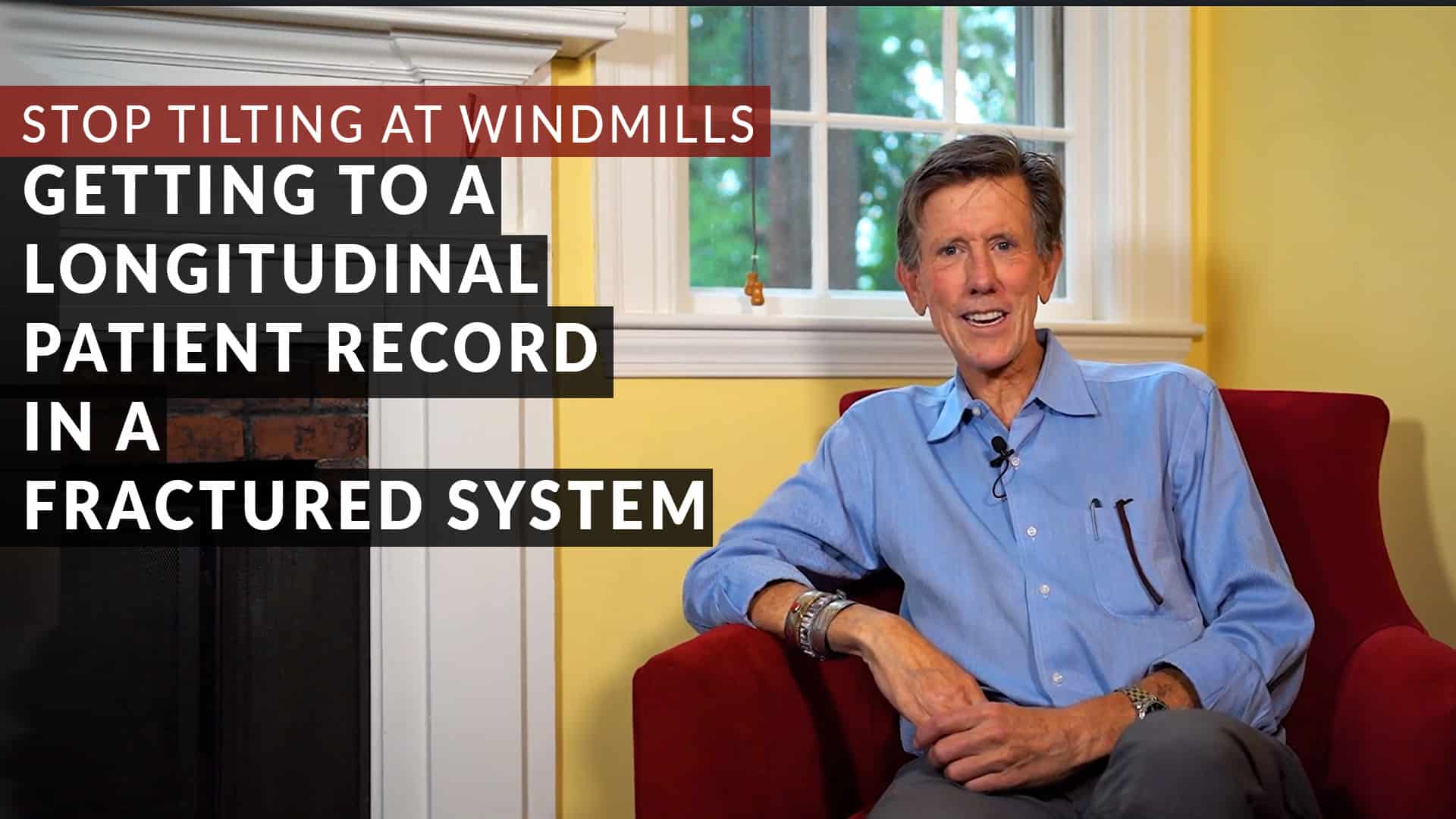
The Need for a Longitudinal Patient Record In A Complex, Fractured System
Being a patient in a fragmented healthcare system is often a tough experience. Streamlining access to data via LPRs is a step forward, but obstacles remain.
Patient Access APIs: Good Intentions Aren’t Enough
In this Hot Take, Brian Murphy discusses the recent Patient Access API requirement from the Centers for Medicare and Medicaid Services (CMS).
Looking to the Future – 2021 Predictions
Unlike past years when we have written a post evaluating how well our predictions for that year...
Building the Care Delivery Chain
This week we learned that Collective Medical will be acquired by Canadian-based PointClickCare for a whopping $650M. That is a phenomenal multiple to Collective Medical’s estimated annual revenue of about $45M. Is it an unreasonable valuation? No, and here’s why.
Take a Break From Worrying About COVID-19. We Have New Rules!
The 21st Century Cures Act said that patients should be able to move from health plan to health plan or from provider to provider and have their data go with them.
Chilmark’s Recommended HIMSS’20 Sessions
Once again, the Chilmark team is headed to Orlando for another HIMSS Global Conference and...
Predictions: What’s in Store for 2020?
As we rapidly approach the end of the year it is time once again to look forward to a new year, a...