
The MU workgroup broke down meaningful use into 5 broad categories:
- Improve quality, safety, efficiency and reduce health disparities.
- Engage patients and families.
- Improve care coordination.
- Improve population and public health.
- Insure adequate privacy and security protections for personal health information.
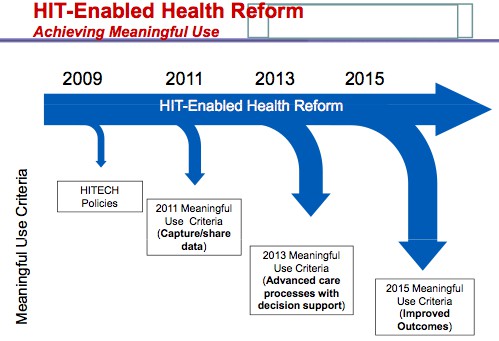
Within each category, the MU workgroup set specific objectives and measures. As proposed, these objectives and measures will ratchet up in two year increments, 2011, 2013 and 2015. In 2011, the broad objective is to capture and share data. For 2013, MU is to advance care processes with decision support. In 2015 MU criteria focus on improving outcomes.
A 7pg MU matrix (PDF) is now up on the HHS site provides a clear picture of what is proposed. This matrix has a significant amount of info, far too much to cover within the context of a post, so please take a look for yourself. Chilmark’s summary assessment:
The Good:
The MU workgroup was charged with an enormous task and have done an impressive amount of work in a relatively short time-frame defining clear, comprehensive goals and objectives for MU. The five broad categories successfully reflect the prime precepts of the ARRA HITECH legislation, going beyond ARRA’s suggestions of meaningful use to address such critical issues such as consumer rights to Personal Health Information (PHI), public health, privacy and security.
The MU recommendations have a strong focus on creating and exchanging data elements that are already becoming “liquid” (e.g., meds and labs) a logical place to start and one that can be accomplished without undue burden. Also, the strong desire on the part o the workgroup to direct MU recommendations towards outcomes and not just focus on technology is to be commended.
The Challenges:
Despite the fine work that has been done the MU recommendations are DOA.
The bar has been set too high and the recommendations put forth will be virtually impossible to implement within the aggressive time schedule of the HITECH Act. Simply put, it appears that not enough attention was paid to the processes/workflow changes that are required as part of a successful HIT roll-out to meet these MU recommendations.
For example, recommendations call for CPOE use in 2011. CPOE is extremely challenging to implement and the technology piece is actually a pretty small component of the overall implentation. The real challenge with CPOE is its direct impact on physician workflow and practices. Thus, CPOE requires significant forethought, process mapping, implementation and training. Getting all that done and to demonstrate meaningful CPOE use by 2011? Don’t bet on it.
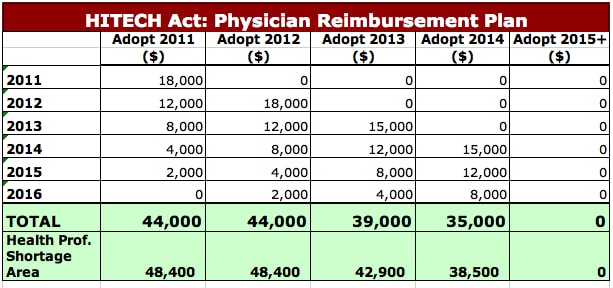
An even bigger challenge may simply be the reimbursement schedule’s structure, especially for those smaller practices who may not derive a significant portion of their payments from CMS and thus not heavily impacted with future CMS penalties. (We do not have to worry so much about hospitals and IDNs as the future 5% CMS payment penalty is more than enough incentive). The reimbursement schedule, which was written into the legislation is front-end loaded, i.e., physician reimbursement higher in early years than later ones (see table). Ratcheting up MU criteria from 2011 to 2015 may make compliance to MU criteria so onerous that physicians simply opt-out of reimbursement in 2015, which for one starting in 2011, only represents a loss of $2,000.
There is also the issue of the technology itself. Will the physician’s EHR vendor be able, or willing to keep pace with this schedule of MU recommendations, will they embed the needed technology in their solutions to assist the physician/practice/hospital to readily meet future MU criteria? Will there be enough good, experienced consultants available to assist with implementing new changes? Sure, the larger EMR providers will be able to do it, and large hospitals and IDNs will be able to get the good consultants, but will smaller providers be able to keep pace? Much of this may be answered in the future in how ONC defines “certified EHR” and what may come of extension centers. If ONC keeps the definition of “certified” loose to encapsulate an ability for a physician to readily mix and match any number of apps to meet MU criteria, we may have a chance, but currently, it does not appear that we are heading in that direction for certification.
The Wrap:
The MU draft recommendations of this workgroup are just that, DRAFT. Discussions today during the HIT Policy Committee meeting were wide ranging and significant. Chilmark also had an opportunity to participate in an ad hoc call this afternoon sponsored by a mid-western IDN’s CIO. During that call as well, discussion was wide ranging, but in this case the focus was more on whether or not the MU recommendations were even doable. Answer was a universal, No and most on this call plan to provide comments to ONC on what is actually doable/reasonable to accomplish within the tight legislative time-frame of the ARRA.
Looking ahead, core MU recommendations addressing privacy and security will pass through with little change. Details regarding “% values” for reporting of various health data metrics will be a key part of negotiations/deliberations. Significant challenges will arise regarding level of CPOE adoption and by who (hospitals vs practices) as well as patient engagement as it pertains to home monitoring with biometrics and eConsult capabilities (2013) and providing PHR with real-time view of EMR data (2015).
Stay tuned folks, it will be an interesting evolution for MU in the coming months.




How will the ad hoc call participants’ “doable” MU recommendations be organized, reconciled with each other, and be made simple “action activities” for providers of all types? (“Simple” as in not “rocket science” that providers will embrace, not shirk.)
Should this be the responsibility of the HIT Regional Extension Centers?
Your tweet brought me here. Thanks!
Kel
Anything is possible with the right approach:
RE: CPOE
I could be wrong, but I think there are several vendors with a strong CPOE track record. Based on KLAS findings, there are three. As such, I have to believe they have found a “process” for adoption, somehow.
Physician adoption may prove a bit more challenging. But if the hospitals are willing to share the experience, at least with referring- and and hospital-employed-group practices, there may be a way for a percentage of these groups (don’t know how large that audience is) to achieve adoption with relative ease.
Would love to hear opinions.
Dan