Healthcare spending in the US continues to grow despite the many recent efforts to curb that growth. It is was over $9,500 per person per year in 2014, up from $8,500 in 2011, and is expected to expand into the foreseeable future. In fact, the Obama Administration, in a report recently published in the journal Health Affairs forecasts spending in 2016 will cross the $10,000 per person level and expand at the rate of 5.8% per year for the next ten years. This rate of growth is nearly double the rate of growth as recently as 2013. Meanwhile economic growth remains stagnant, with household incomes nearly equal to the spending for healthcare alone.
Attribution for this growth in spending is laid on many factors, some spurious. These include: an aging population; more coverage under the ACA (but the uninsured only decreased from about 10% of the population to about 9%); inflation (which has been nominally nil); and more expensive treatment regimes. What is missing from this list is the enormous increases in administrative and regulatory burdens placed on providers.
Our recently released Chilmark Research Insight Report, Making Healthcare Affordable: Implementing True Continuous Costing, takes an unvarnished look at how much we really spend on healthcare, where the money comes from and where it goes.
The inescapable finding in the report is that to make healthcare more affordable we first need to reduce the real costs of healthcare, which are the actual true costs providers incur when delivering healthcare services.
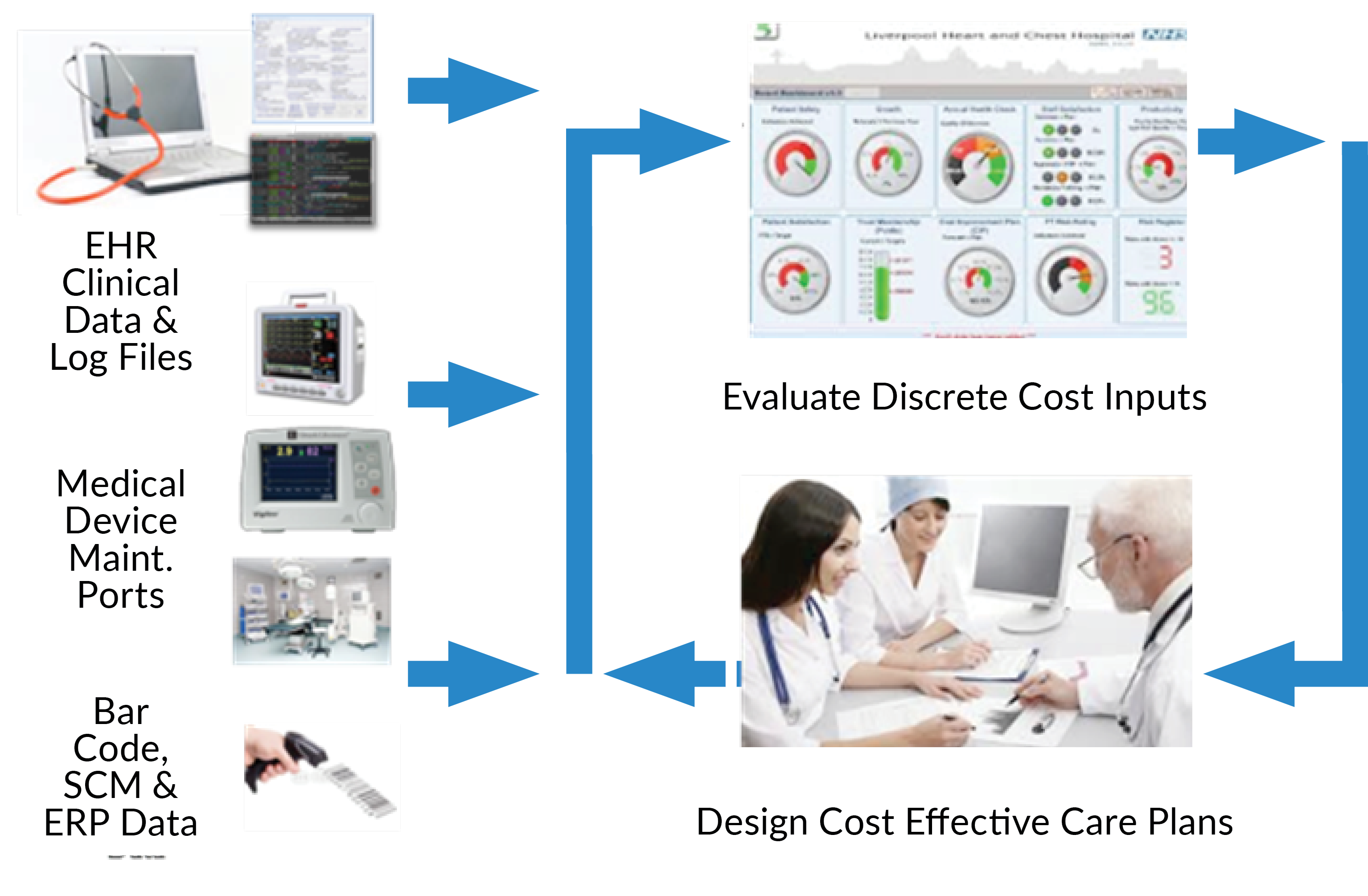
The report introduces what we call True Continuous Costing and lays out a simple and effective plan for measuring, monitoring, and managing the cost of care using data already inside provider organizations. It also deals with common objections to implementing cost controls and provides a roadmap on how to succeed.
True Continuous Costing uses modern analytics combined with data providers already have to measure, monitor and manage their costs of providing care on an encounter by encounter, patient by patient, and minute by minute basis to assure they are delivering services at the lowest possible cost.
Sadly, our research indicates that few providers can tell you with precision how much cost variability they have in similar admissions, procedures, tests, or anything else. This is unfortunate given the widespread availability of technology, the ubiquity of true cost data at every provider, and the very nature of the healthcare business.
Until you understand your costs you cannot do anything about them. As has been stated numerous times in the past, the first key to improvement is measurement.




I agree completely with Rob. Despite our investments in healthcare transformation from the Affordable Care Act and the HITECH act, our average per capita cost for healthcare in the US is still going up. We will crack the $10,000 per capita mark this year. It’s beyond me to understand how we can expect to reduce the cost of care when we have almost no clue about our current cost of care, on a specific patient basis; it’s all very smeared averages. We all know that the charge master is a joke. We all know that it needs to be converted into a cost master, like the rest of the normal business world operates. We have even fewer clues how much money we need to invest to achieve a unit of outcome improvement for a patient– a concept that I call Return on Engagement (ROE). As a national policy strategy, we’ve completely missed the target in terms of understanding our costs and reducing our costs. Vendors need to produce better products and systems to support cost accounting and healthcare leadership needs to embrace detailed cost accounting as a imperative priority. Rob is a great thinker in this topic area and his concepts are right on target.
Thanks Dale,
I am struck by how few providers pay attention to costs. They have all the data they need. The technology is very mature and relatively easy to use. There is clearly ROI upside. But what I find most curious is lack of interest. I am a member of the HFMA Florida Chapter and have offered my services free of charge over and over to providers all over the State to come in and kick start a project to help them identify and analyze patient specific costs. So far crickets.
Rob