Pandemics are by definition a global issue and it is in the interest of all nations to pay attention to the global response to the emerging COVID-19 outbreak. This is not a time for myopic views or “America First” at the exclusion of learning lessons in real-time from what is going on in contexts as far off as Africa and Asia. Furthermore, part of responding to the immediate crisis entails building the critical infrastructure and cooperation that should have been in place in the first place given the warnings that global health experts have been providing for over two decades.

A Brief Detour into Past Frameworks for Preparedness
In 2018 Nathan Wolfe and colleagues from Metabiota, a company focused on disease surveillance and risk management related to pandemics, created an Epidemic Preparedness Index (EPI) in order to assess national level preparedness. The EPI covered 188 countries and had five indices of preparedness:
- Public health communications
- Public health systems
- Institutional capacity
- Economic resources
- Infrastructure
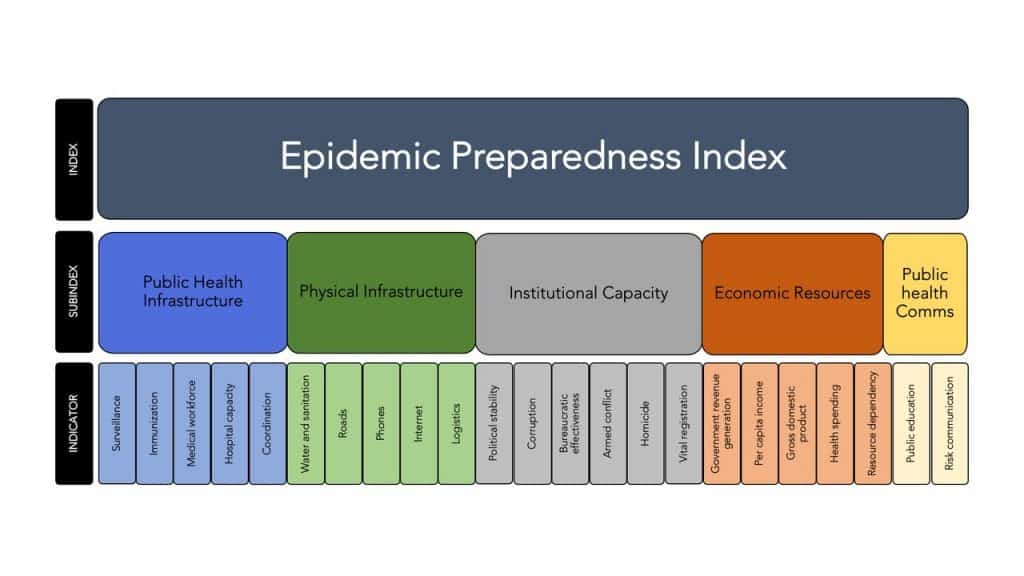
The EPI captures the factors that affect the ability of health and governmental institutions to detect, report and respond to outbreaks. From our experience to date with COVID-19, EPI provides an analytical framework to understand relative rates of growth in different national contexts where we are seeing dramatically different curves for death rates and prevalence rates over time.
Overview of Country Responses to COVID-19 January-March 2020
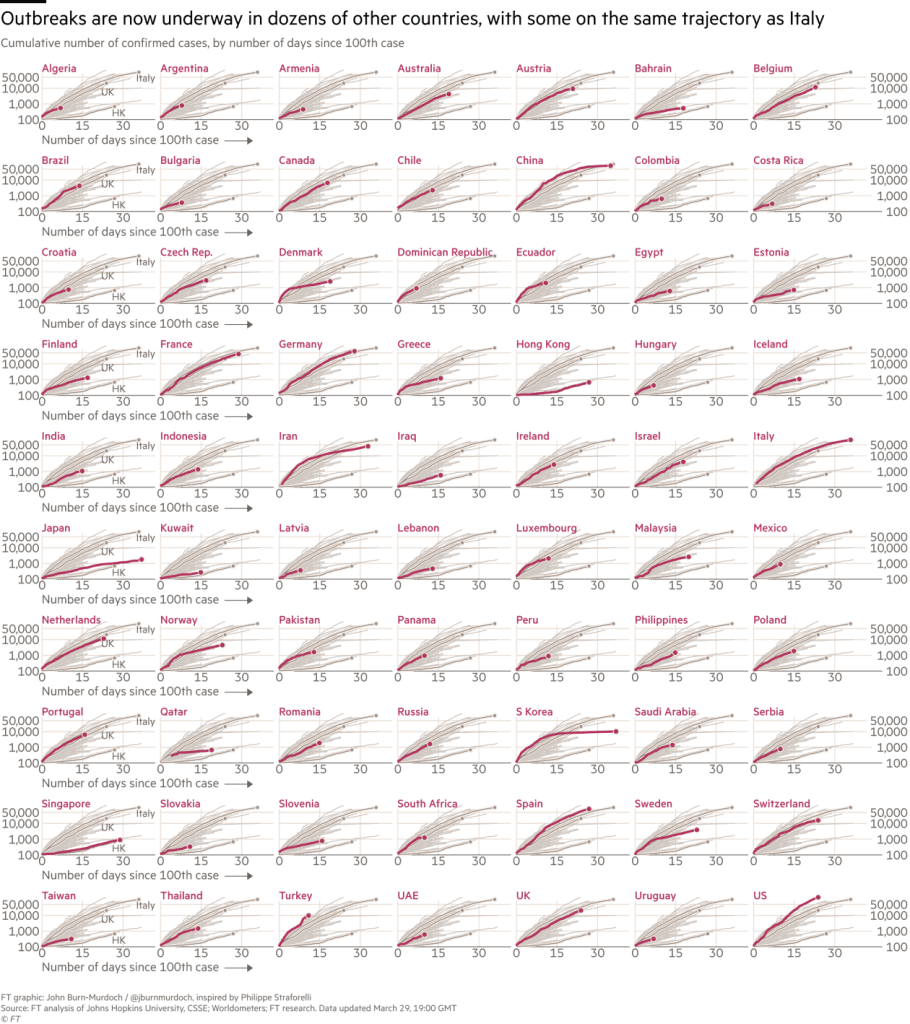
The Financial Times (UK) has been generating useful charts for comparing trajectories across countries. While many countries are still in the early days so the slope of their curves may be somewhat misleading, we can still see dramatic differences in countries that were prepared for the outbreak and those that were slow to act.
One of the most interesting examples is Taiwan. On December 31, 2019, at the moment China notified WHO of pneumonia cases of unknown origin, Taiwanese health workers boarded a plan to Wuhan. Early models predicted that Taiwan would be one of the hardest hit due to the proximity to Wuhan and the number of daily flights from China. As of March 23 they had 195 cases total and may be in the early days of experiencing a second wave after initial lockdown/shelter-in-place efforts were mildly loosened. How did they successfully manage to contain the outbreak in ways that most of Europe and the US have not?
First, Taiwan learned from the SARS epidemic in 2003 and created the National Health Command Center to manage large outbreaks. This is the cornerstone that enabled a centralized command center for identifying cases, instituting containment strategies and resource allocation. The national health insurance database was rapidly integrated into the immigration and customs database to enable real-time data analytics capabilities that could identify high-risk travelers. A QR code scanning capability and online travel history and clinical symptoms system enabled alerts. SMS codes were used at customs checkpoints for faster immigration clearance and identification of high-risk patients based on travel history and symptoms who could be immediately quarantined and tracked through their mobile phones.
The Taiwan Centers for Disease Control also coordinated multiple ministries including transportation, economics, labor, education and EPA for comprehensive strategies to contain the virus. They were able to coordinate prices for surgical mask production and allocation, for example. These efforts were coupled with a clear and comprehensive communications strategy from central government authorities where the economic impact, effects on education and issues like hoarding were addressed early on.
While we hear much about South Korea’s example of scaling up of testing to control the pandemic, Taiwan is a good example of a well-coordinated public health approach empowered by data analytics, inter-sectoral collaboration and testing targeted in a proactive way before the epidemic got out of hand. Their actions were quick, decisive, and well-coordinated.
Rwanda, a Low-Income Example with a Solid Health System
A very serious concern is how low-income countries will confront the COVID-19 threat with limited resources. This should be a concern for all of us since this is a global concern that can rapidly cross borders. It is in every nation’s interests that the pandemic is controlled in Africa, Asia, and Latin America. By March 19, 2020, African countries had reported more than 600 cases and 17 deaths according to WHO.
Rwanda has gained a great deal of attention in global health circles over the past decade for its public health efforts. A drone airport exists to send medical supplies across the country. A well-functioning health IT system exists and they have dramatically improved coverage of AIDS anti-retrovirals.
Taiwan and Rwanda provide examples illustrative of the impact that preparedness and investing in scalable, interoperable health systems can have during a major public health emergency and how preparedness saves lives.
On March 21, Rwanda became the first country in Africa to impose a lockdown after confirming 17 cases. The lock-down included a ban on unnecessary movements and visits outside of the home, encouraging electronic payments, all public and private sector employees to work from home, closure of borders, closure of markets and banning of motos for transportation. Returning citizens from abroad are put under 14-day quarantine. Restaurants and cafes are only allowed carry-out. There were soon reports of arrests of those attending worship services.
Rwanda very rapidly installed public handwashing stations throughout cities and towns in front of shops, restaurants and bus stops. Nearly 500 health workers were rapidly trained to monitor body temperatures, conduct health communications and address other containment measures in an expedient manner. It is important to note that a quarantine in the context of Rwanda that lacks financial resources for bailouts of citizens and small businesses will be an interesting example to watch for the political fallout. President Paul Kagame has been known for his use of authoritarian measures when viewed as necessary to maintain the peace since the genocide of 1994. How long Rwandan households can maintain a lockdown and survive the crisis is an open question.
These two examples are illustrative of the impact that preparedness and investing in scalable, interoperable health systems can have during a major public health emergency. They also clearly illustrate that in times of a pandemic, having a clear command center strategy with quick, thoughtful and decisive leadership at the helm can mean the difference between a full-blown outbreak, as we have seen in Italy and now in the U.S., and or much more contained outbreak as in the case of Taiwan, Rwanda, and South Korea. Granted, the US is a much larger country by far. Nevertheless, preparedness saves lives.
NOTE: As part of Chilmark’s response to the pandemic, we are curating a list of free health IT resources available to the public. If you know of something we missed, please let us know!




0 Comments