How APIs Can Bridge the Gap Between Organizations’ Data Systems

As healthcare evolves, driven by technological advances and transforming patient expectations, patient engagement has emerged as a critical strategy for providing high-quality, patient-centered care. Patient engagement significantly impacts patient outcomes, which has become increasingly important in healthcare as quality-driven payments and capitation models grow in volume. Patients who are engaged and take the driver’s seat regarding their healthcare are more likely to make informed decisions, adhere to treatment plans, have an overall better experience, and have higher levels of satisfaction with their healthcare.
By empowering patients to take charge of their healthcare, we are one step closer to creating a more patient-centric healthcare ecosystem. So, why not engage from the device that’s glued to us 24/7? This is the goal of the December 6th CMS proposal, requiring payers to use the health information technology (IT) standards at 45 CFR 170.215 that are applicable to each set of API requirements proposed in this rule, including the HL7 Fast Healthcare Interoperability Resources (FHIR) standard (CMS PDF on proposed rule).
Professional Groups Advocate for Accelerated Enforcement Timeline
Healthcare and technology organizations are pushing for healthcare providers and payers that are actively participating in Medicaid and Medicare programs to utilize open APIs to grant patients access to their data via a third-party application of choice. The Medical Group Management Association (MGMA) and the Workforce for Electronic Data Interchange (WEDI) call for the CMS provisions to be enforced before the proposed date of January 1st, 2026. Their specific rationale for expediting this enforcement? To enable more seamless and less disruptive prior authorization protocols – though the benefits go well beyond this important business case.
Efficient and transparent prior authorization processes are crucial for improving patient engagement and outcomes. Proposed interoperability and prior authorization rule changes offer significant benefits in this regard. By leveraging technology and API integration, providers can streamline their prior auth processes, saving valuable time and resources that can be better allocated toward patient care, without causing as much disruption for the patient. By emphasizing the connection between efficient prior auth and better patient experiences, healthcare and technology groups can promote the adoption and support for these critical changes despite expected pushback from payer organizations who utilize prior authorization schemes to manage member utilization.
The proposed rule is necessary to drive interoperability and streamline data exchange between traditionally contentious payers and providers, ultimately reducing the administrative burden on care delivery organizations and ensuring they have access to up-to-date health information. The new rule must also implement changes to the prior authorization process, including increased transparency and standardization of requirements. The proposed rule is a crucial step forward in improving the efficiency and effectiveness of the healthcare system, and its implementation is critical to helping contain the growing costs of care delivery in the US.
This call to action would enable patients to oversee their healthcare more directly by allowing them to easily access and share their health information with various providers and caregivers. In addition, this would also hold healthcare providers accountable for electronically sharing admissions, discharge, and transfer (ADT) data with other providers, as well as post electronic patient event notifications to notify providers when an ADT is logged.
The aim is to guarantee that providers can access up-to-date patient information. This allows them to make informed clinical decisions while improving collaboration amongst healthcare stakeholders and encouraging coordinated, patient-centered care. This proposed rule would prohibit information blocking, defined as:
“Business, technical, and organizational practices that prevent or materially discourage the access, exchange, or use of electronic health information (EHI) when an Actor knows, or (for some Actors like EHR vendors) should know, that these practices are likely to interfere with access, exchange, or use of EHI. If conducted by a health care provider, there must also be knowledge that such practice is unreasonable and likely to interfere with, prevent, or materially discourage access, exchange, or use of EHI.”
This enables the breakdown of barriers to health information exchange, improving collaboration between different healthcare stakeholders and enabling more coordinated, patient-centered care.
While there are mandates relating to interoperability coming out seemingly every day, this one is significant. In order to meet interoperability demands, Drew Ivan, Chief Strategy Officer at Rhapsody (née Lyniate), asserts that health systems, payers, and providers must “get good at APIs and do more than the minimum required to meet compliance. Healthcare organizations need to take control of their data.”
The Growing Import of APIs to Drive Interoperability
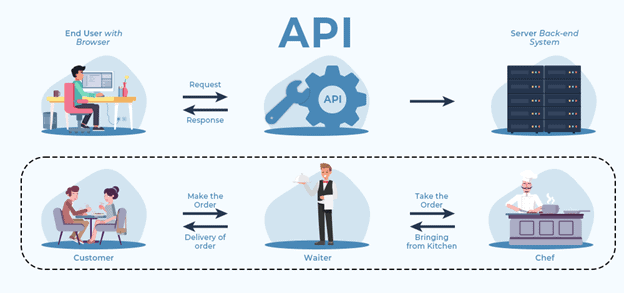
For the last decade, the Office of the National Coordinator (ONC) has been discussing an interoperability infrastructure built on the backs of APIs that use common, accepted standards such as FHIR, CDA, HL7, X12, etc. APIs are already playing a critical role in achieving the nationwide interoperability we strive for by enabling various software systems and applications to communicate with each other, granting them the ability to exchange and share specific data elements seamlessly.
The impact of APIs is felt across all tech-enabled industries, including healthcare, finance, and logistics. In healthcare, they provide a secure and efficient way to exchange data between providers and patients. Third-party applications can allow patients to access their health data via preferred modalities such as mobile apps or other digital tools, which can help them manage their health and communicate with healthcare providers. In addition, APIs connect healthcare providers with public health agencies, enabling real-time disease surveillance and outbreak response (when it works).
Some notable healthcare API players include the varied purpose-built integration and API vendors like Flexpa, Redox, Moxe, Health Gorilla, Particle, 1upHealth, Validic, and Zus (to name just a few we’ve spoken with recently), as well as the big EHR vendors (Epic, Oracle Cerner, athenahealth, etc). Writ large, these companies provide APIs that enable streamlined data exchange, secure data sharing, and interoperability between healthcare providers and patients.
Speaking of Epic, this week saw a cohort of 22 notable Epic clients sign on to TEFCA, a potentially monumental step forward in the healthcare industry. This should improve interoperability and data sharing among healthcare providers, leading to better patient outcomes and a more efficient healthcare system. With the support of such a powerful consortium, TEFCA is poised to become a dominant force in the healthcare industry. It will be captivating to witness the progress of this partnership and the groundbreaking innovations that will ensue.
Closing Thoughts
By utilizing APIs, healthcare organizations can make workflows more efficient for providers, reduce healthcare costs, and improve patient outcomes. Via these third-party apps, patients can monitor their health status and medication adherence and communicate with their healthcare providers effectively, leading to better health outcomes and increased patient satisfaction.
In an era molded by technology, APIs have become critical gateways of communication. APIs are valuable resources in our trek to attain seamless interoperability amongst varying systems and applications; integrating APIs in organizations that rely heavily on interconnected technology ultimately drives innovation. By providing standardized models for data exchange and communication, APIs enable seamless communication, enhancing organizational processes and maximizing system efficiency.
Grab a free download of this report below!




0 Comments