A recent report has gone great lengths to explain how and to what extent telehealth can improve outcomes, and it is well worth a read if your healthcare organization (HCO) plans to explore investments in telehealth services now or in the future.
No, I’m not talking about The Wall Street Journal declaration that telemedicine is transforming healthcare. The top-fold placement of the story was indeed nice, as was the accompanying interview suggesting that technology in general can improve population health, but the article wasn’t exactly news to the healthcare industry. (Not to sound like a hipster, but I wrote my “telemedicine is changing healthcare IT” article back in 2012, before it was cool.)
As it turns out, the report in question is a technical brief from the Agency for Healthcare Research and Quality (AHRQ) that examined 58 research studies to find evidence of telehealth’s effectiveness across both clinical areas and technical functionality. In a nutshell, the interventions with the greatest impact on outcomes tend to target chronic conditions.
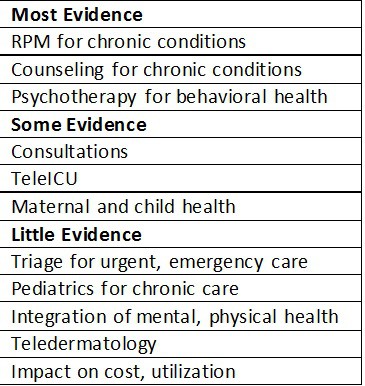
The table at right summarizes the findings. Here are four additional observations.
- AHRQ defined telehealth as “the use of technology to facilitate an interaction between a patient and the healthcare system or interaction between two or more providers when the interaction was directly related to an individual patient’s care.” The key phrase there is healthcare system, as it implies that a relationship between the patient and the HCO already exists. This strikes a blow to direct-to-consumer apps, but it also indicates that creating yet another siloed venue of care won’t benefit patients or providers.
- To treat Type 2 diabetes, communication and counseling work well, but RPM does not. This makes sense. The Diabetes Prevention Program (DPP) model, which the Centers for Medicare & Medicaid Services (CMS) wants to take national, emphasizes counseling in the form of weekly in-person group visits, with topics such as barriers to healthy eating and physical activity. Monitoring, on the other hand, serves as a constant reminder to someone that he or she is sick; it’s not a tool for motivating behavior change.
- In the words of AHRQ, RPM is an effective use of telehealth because “it makes new or significantly different forms of information and treatment available that can supplement and extend office-based care rather than replace face-to-face interactions.” Simply changing the mode of care delivery isn’t enough to improve outcomes. Telehealth must change the form of care altogether. This should offer pause to any payer, provider, or vendor that thinks simply digitizing an in-person care encounter will flip the healthcare industry on its head.
- Chilmark Research usually advocates faster adoption of technology as opposed to perpetual pilots, but any telehealth use case that hasn’t had a demonstrable effect on cost and utilization – we’re looking at you, teledermatology – should be subject to scrutiny. Take tele-triage: Does it direct patients to the most appropriate care setting or, in the absence of licensed medical professionals and/or evidence-based protocols, does it just funnel patients to the ED?
Teladoc’s recent, pricey acquisition of HealthiestYou begins to confirm our prediction that the telehealth market is ripe for consolidation. As the moving and shaking continues, HCOs must avoid the perils of shiny objects that address single episodes of care and instead seek telehealth partners that improve outcomes for chronic patients while controlling costs. The former will make headlines, but the latter will transform healthcare.




Its been our experience that BOTH Telehealth and Telemedicine are simply TRANSFORMING healthcare as we know it… And for good reason. We find in our own practice that servicing MORE patients with quality analysis from a Doctor (even if via teleconference) has several benefits: 1) Patients sanctification ratings are higher (as they are NOT only being seen by physician assistants and 2) We can see a greater volume of patients without having to PHYSICALLY be in multiple locations.
Great job on this write up! Great to see some actual data for a change and not the fluff from a WalStreet editorial =0)
Thanks for the feedback and real world experience. And agree, much of what one reads in the press is far from portraying an accurate picture of what is really occurring in the industry. Lazy reporters or just lack of knowledge and nuances – likely a little of both.
I’m excited for all these recent changes to medicine. We recently got a 24 hour, freestanding ER in Dallas and it is absolutely amazing. We can get the same level of care as a hospital ER without having to wait hours. I’d definitely be interested in this “telemedicine” though, I’d love to be able to skip trips into town for minor medical needs!