Before entering the convoluted healthcare IT sector, I had worked in the manufacturing sector both as an IT analyst and in corporate strategy for Europe’s second largest enterprise software company. In those many years I learn quite a bit about not only how to effectively deploy large enterprise software systems (SAP, PeopleSoft, i2, PTC, SSA, Dassault Systemes, etc.) but how to create models that would guide clients in a methodical manner in IT adoption. A common model used was the five stage Maturity Model, which was originally developed at Carnegie Mellon University.
The beauty of the maturity model is its simplicity and focus on process change. This proved very effective in educating all stakeholders within a manufacturing company, from the C-suite on down, as to how they needed to think about their internal processes, the technology they were preparing to deploy and the final end-point that they should strive towards. But one should not look at maturity models as completely static for the technology does change overtime and subsequently what is possible.
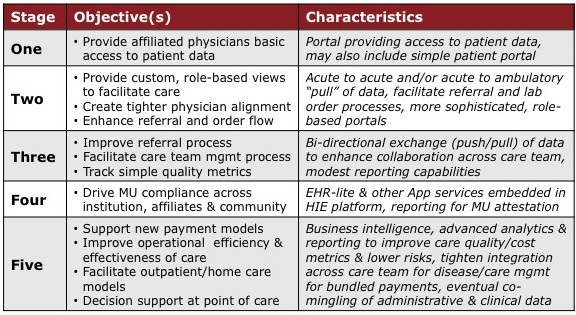
In doing research for the HIE Market Report I was surprised to not find a maturity model for HIEs (heck, it was hard to find much of anything with regards to maturity models in HIT). This puzzled me greatly for if any sector of the HIT space needs a maturity model, it certainly is the HIE sector. This pushed me to create the five stage HIE maturity model shown below. In viewing this model, keep in mind that the model is not meant to be an exhaustive list of all that is possible but simply describe what are the natural characteristics of an HIE as it matures over time. As in the models I created for the manufacturing sector, this one is designed to assist those who are planning to deploy an HIE, or may be operating one now, on what they need to think about in mapping out their future strategy. For this particular model, I used three instead of the customary two columns with the third column (Characteristics) providing guidance as to the IT capabilities that would be required to meet the Objectives of that particular Stage.
What’s next?
Ideally, this maturity model sees wide adoption and use by both public and enterprise HIEs. Honestly, that is why I’m pulling it out of the HIE Market Report and putting it out here in the public domain for part of the mission here at Chilmark Research is to indeed facilitate the effective adoption and use of HIT by ALL stakeholders in the healthcare sector.
Secondly, this is being released to get the feedback of those in the field that are deploying HIEs, running HIEs, providing HIE solutions. Please provide your views, your perspectives on this model. Is it logical? Does it make sense? Is there anything missing?
I look forward to your critque.




John,
Great first-cut – especially for an industry with a rich (and failed) history of trying to “boil the ocean.” My one (small) suggestion would be to exclude the “simple patient portal” altogether (for now). IMHO – what we have in that category today isn’t simple – and is so fractured as to be unusable
Almost every Practice Management/EHR system has a “Patient Portal” and while the other side of the equation – the PHR – may not be a complete failure – the total adoption rate of ~7% is still very low (especially as any kind of model for a single solution).
Just today, a major publication advocated Google abandon Google Health entirely. Dossia (after 5yrs) can measure adoption in the 1,000’s and Revolution Health completely closed their PHR last January. Perhaps the brightest single model is the VA – but then that’s really just a very large “walled garden.”
I think we’ll see more pronounced consumer engagement in time – and we’re all advocating patient-centricity – but it’s just a little too early to actually bake in (IMHO).
:dm
Dan, Would you provide a reference to a major publication advocated Google abandon Google Health entirely. From my point of view, I agree. Google, at a minimum should correct some of the issues like invalid CCR and compliance issues.
Link here: http://read.bi/h7GFMs
Article was titled : 8 Google Products Larry Page Should Kill
# 4 Was Google Health (and I thought the assessment was pretty accurate)
Health: Too much Work, Too Little Reward
“If Google Health really made it easy to organize your medical records in one place it might be useful. But right now it only supports automatic imports from a handful of other online sources, and entering information manually is a huge chore — do you really want to spend your weekend entering your health insurance information into a Web site when most of it is probably in your insurance provider’s site already? Google Health is not going to revolutionize the health care industry and it’s way outside Google’s core business.”
John,
Thanks for sharing this. I have been enjoying your blog and the public facing portions of your work.
I’ve been focused on 5 for quite some time–having dealt with 1-4 for many years, but my personal desire to improve the function and cost of healthcare (and by extension quality for more people), has collided with systemic structural problems.
In other words, the structural integrity of the HC system is defending against anything but a bigger piece of society’s pie, which clearly isn’t sustainable. Given the uncertainty of the political and economic situation surrounding HC in the U.S., and my own experiences, I do not yet see genuine interest in bringing efficiencies to the system– where it matters.
With my old consultant’s hat on from decades past, I have closely observed, audited, and engaged with similar systems, albeit on a much smaller scale than say the entire U.S. HC system, although I have invested considerable time studying it. What I see in HC now is a determined cultural effort to take down the entire system– I do not believe that it’s intentional; rather like so many environments I audited when a younger consulted that were dysfunctional, it’s based primarily on ignorance– not in medicine in this case, but sustainable economics, and each partner’s role within the system.
So while these five are very important– especially the 5th, it may not matter much until the structural issues are dealt with in the HC eco-system. While my experience suggests that most of the people in HC have integrity, the system itself doesn’t, inviting all kinds of misalignment of interests. Treating symptoms can be a lucrative business in the short term, but it doesn’t cure the patient. Thanks for sharing, MM
John,
More generally – I would have to agree with Mark’s assessment as well. We’ve been living with mis-aligned incentives for years. Best comment I heard at an event last week was: “MU is the appetizer for payment reform.”
:dm
Dan,
A patient portal can be useful if it has the types of tools a consumer/patient wants and needs to more effectively interact with their physician. You mention the VA’s work but not KP’s. Kaiser has done tremendous work and now has adoption of their patient facing site at some 40% of all members. Unfortunately, most providers/HCOs do not spend the time or effort to build out truly effective and engaging patient portals, thus the poor adoption.
We have to start somewhere and my real fear with all the $$$ being pumped into the HIE market via HITECH is that the consumer/patient will be ignored. The HIE Working Grp of ONC has all but ignored the consumer in their policy deliberations – a sad state of affairs.
Mark,
The HC market is definitely one of the stranger, more preverse markets that I have ever studied/worked in. And in this market, there is so much $$$ being made on the inefficiencies that no one want s to give up what they currently have despite the fact that on its current trajectory, HC could literally break the bank especially giving the alarming epidemic in chronic disease that will only get worse as baby boomers age.
But I do have hope in that many see HC spending as unsustainable and are looking to change the models of payment. How successful these will be remains to be seen, but I do see promise in bundled payments, shared risk and making the patient/consumer a far more active participant on the care team.
John,
Point taken. KP has done some really excellent work engaging the consumer (Leapfrog gave 16 of the top 18 slots to KP Hospitals in their recent ranking. Footnote: Mayo here in Phoenix was #1).
But … KP is more like Dossia than VA (a relatively large “walled garden”). It’s great as long as I stay in that system – but like all “patient-portals” – I bear ALL the risk of portability outside that system. That’s a really poor design – and interoperability there feel a lot like the Bataan death march.
Welcome the chance to chat more on this – it’s an area I’m actually working on with ipatient.
:dm
Couple of points Dan:
First, Dossia fully supports portability of a member’s PHI, thus not truly a walled garden. The challenge they face is creating an ecosystem that is vibrant and useful enough for their members (employees of large self-insured companies) will want to use. Unlike KP’s MyChart that allows members/patients to conduct transactions, which has proven to be most desired by consumers, Dossia has very little in support of transactional processes. Still very much a work in progress.
-John
John,
Portability isn’t the objective – usability is. Almost any system allows for the easy export of data. The issue is where can that be imported? Assuming there’s an EHR (not reasonable yet) – almost nowhere – and as a consumer/patient that risk is 100% mine. IMHO – easy/best to revisit the patient side once we have more of the EHR/HIE equation at least functional.
Dan,
> Portability isn’t the objective – usability is.
That’s in the eye of the beholder, eh?
I want both – we MUST have both. But I don’t see any reason why portability should wait for usability.
btw, the Data Portability project is developing lots of practices around portability (not specific to healthcare).
On another note, to my knowledge it’s not at all accurate that almost any system allows for easy export – and besides, as you say, the issue is who could read it in.
Dave,
I think both (portability and usability) are minimum requirements.
Portability is a lower barrier technically (relatively easy for a vendor to mechanically export their data to something). They may not want to do that – but that’s a different issue. The heavier lift is where can I go with that (as I think you discovered with your records earlier in your experience?). That’s really what I meant by usability. As I understand it – when you did (finally) get your records (into Google?) – they were pretty useless.
In the absence of reasonable usability – most consumers aren’t interested in portability alone. That’s the risk I was referencing – and what we’ve also seen in the market with Google Health, Dossia, MSFT HealthVault, Revolution Health etc….
I do see options/solutions ahead – and we’re working on a contribution in this area as well. Welcome the chance to show you anytime.
:dm
@danmunro
John,
I like what you’ve written, but you will have to change it in a few years (at least I hope so). See my critique
Keith
We may not have a few years Keith — enjoyed your critique btw. In studying macro economic systems, and combined with many other factors–sharing tech trends, cultural shifts, wealth movement–I truly don’t believe we have much time at all. HC reform needed to happen long ago.
I hear you John — much the same in many other areas of our economy– just none as large and growing in as ill health–finance and government aren’t doing terribly well either, but they are connected.
I view HC similar to many physicians and teachers– that it’s foundational– nothing more important. We part ways when everything else, including their system, depends on their system improving radically, but none are willing to accept. Unfortunately, a rather long history of case studies in less entrenched industries with less systemic dysfunction (economically, organizationally) have demonstrated pretty clearly that change will only occur when left with no other choice (whether by competition, economics, or regulation). The UK is actually kind of interesting now as one attempting to radically reform without being forced. We’ll see if their outcome is any different.
I agree that patients need to be not only part of the team; indeed I am quite certain they need to be the leader. In many personal experiences now, those who took control and became expert in their own health have done much better than those who relied on the HC system. This includes close friends and family with ALS, Diabetes, stage 4 cancer, MS, and disabling back pain, among others.
I wish I were as optimistic as you guys– probably reflects the perspective– we don’t have sufficient incentive to invest in providing improved efficiencies. As I see it the risk/reward equation is still very much tilted towards becoming part of the problem rather than the solution.
Experiments and modeling can work–particularly in real-world environments, but only when parties are serious about adopting improved innovations– otherwise they tend to be reverse engineered for defensive purposes, which I see evidenced in the logs of downloads in our own scenarios. As it stands now most of what I see in HC on the economic modeling side is defensive, with primarily disincentives for problem solvers.
One hint that needs to be widely understood about innovation — those who are the problem rarely provide the solutions. My confidence lies not in the political system at this point, but rather attempts at entirely new models outside of the diseased body of the HC system. .02-MM
FYI only.
KP’s Phil Fasano talks about the worlds largest EHR implementation (HealthConnect) in the Feb edition of InformationWeek/Healthcare – http://bit.ly/g2oWzR
“Much of the progress Kaiser Permanente has made in recent years in population care and care registries is a direct result of fluid information exchange among providers—and between
providers and patients.”
Thanks Dan, that’s a great quote!
> it was hard to find much of anything with regards to
> maturity models in HIT. … This puzzled me greatly
> for if any sector of the HIT space needs a maturity model,
> it certainly is the HIE sector.
Well, dat’s kinda what I been tellin’ you since I first noticed you. Except for me it was a gut feel, based on other industries, and you’re able to articulate it.
And yeah, I’ll echo Dan’s original comment about boiling the ocean. Thanks to all for giving me a way to express what we need to do. Looking forward to seeing how this unfolds.
I am a entreprenuer of a House Call Physicians Network, a major in the Air Force, a veteran, and also a past VA physician who has experience in the VA system as both a patient and HC provider. Really, i have not seen one HC system with the same capability like the VA (probably with the exception of the Military), at least of 6 other major systems i have experience with (i.e. AHLTA, Cerner, Practice Fusion, etc). I don’t have the experience with Epic and Mayo yet, but VA still has the best model in term of cost and efficiency. Too bad it’s has not been customized effectively for civilian sector….. Imagine you can create a civilian super primary care model without VA’s wall. Would that be impressive. John, i think your 5 steps are great, but one does not have to follow one at the time, especially they use VA’s platform. An innovative business model should not limit itself to the MU, but should do what best fit into current business model, then implement the rest at a later time when the business model and constant HC changing environment warrant specific step, including MU. Therefore, it may not happen today, but may happen 3-5 years down the line in the software development planning. I wonder if you interviews with the executives for HIE have included a review of their corporate 5 years HIT planning or not??? I doubt it. Anyhow, it’s just my 2 cents opinion….. LCN
Thanks for your comments Linh. Agree with most of what you stated, much of which is included in the HIE Report. For example, the report provides a comparison of needs of enterprise vs public HIEs and there are some distinct differences driven by economic/business needs and not MU alone. The Maturity Model was developed based on the core commonality of needs across all HIEs, regardless of sponsor.
And I sincerely appreciate your “2 cents opinion.”
-John
In the NHS we have had several HIT maturity models based on the functionality available in EMRs.
The problem with them, and with this one, is that they don’t align with the value that clinicians want. For example, in a project I am working on currently clinicians say that Point of Care DSS is very important to them. We may say (correctly from an architectural point of view) they have to wait until their systems get more sophisticated. But this may mean that clinicians will not engage until the maturity model aligns with their value model.
Great point, Ben. I’m all in favor of systems being useful for the people who need to use them.
Has anyone proposed a model developed from that perspective?
If it’s not possible (for the reasons you cite), perhaps analysts could add columns for each phase identifying when to expect a favorable response from each stakeholder, hm? That would help managers (and the stakeholders) understand during an implementation whether things are going as one would expect.
Ben, you make an excellent point, but therein lies some of the friction in our HC system.
Simply put, there are so many players/stakeholders and each wants their say, things (IT adoption) to work in their favor. For example, Stages 1-3 are really about first trying to get information out to affiliated physicians quickly, in public HIEs to improve community health, in enterprise HIEs, to improve order/referral flow back to the sponsor (anchor hospital). In public HIEs, they have struggled to define a sustainability model outside of grant funding with little success (docs don’t see a lot of value). Enterprise HIEs have, by and large, done fairly well generating an ROI for the sponsor.
Point of care DSS is where both Enterprise and Public HIEs want to get to, but getting there requires a basic backbone for information flow, something we still don’t have here in the US, not even close.
Ben – your point …
“The problem with them, and with this one, is that they don’t align with the value that clinicians want.”
.. is the same one on the consumer/patient side. We have not really found a consumer value that’s high enough to get really large adoption.
I’m NOT advocating that we abandon hope – as much as double-down with new bets on new solutions. Let’s invest in the startup ecosystem – liberally. Two things will happen. 1) We will arrive at solutions. 2) Incumbent vendors that DON’T pivot – will lose market share – and get left behind.
Footnote. There was a significant announcement on Friday in Silicon Valley. Yuri Milner and Ron Conway (serial angel investors) announced that they were going to fund the entire Y-Combinator class (40 startups) with $150,000. The article is here: http://tcrn.ch/e2fDsg
I applaud their vision. Now if we can just copy that model in healthcare 😉
:dm
In a nutshell, the more I read about HIE the more I don’t understand what it is.
Is HIE a user accessible product, or is HIE a backend function of user accessible products, such as EHRs or PHRs? And by user I mean providers, patients, payers, regulators and all other human stakeholders.
My gut feeling is that the latter is a more accurate way to look at HIE, in which case many of the functionalities in this CMM belong to the EHR/PHR which utilizes HIE.
I have to admit that I am a bit puzzled by the various HIE companies, and HIOs who use their products, trying to pretty much compete with EHRs instead of concentrating on providing services for EHRs.
The other portion of this endeavor that I find confusing is the assignment of functionality to specific goals. Most often we say that we are aiming at improving patient care and making it more cost effective and some (myself included) would add improving population health. Everybody can agree with these nebulous definitions in principle, but when it comes to measuring, and we must measure, there really is no agreement on how better patient care should be represented by measurable events, or what measurable activities are prerequisite to better patient care.
Here is where I have to agree with Keith that a CMM should probably stay away from specific functionalities at this point.
My 2 cents…..
Why do so many HIE models exclude the consumer? If the point of the HIE ultimately is to improve access to records, increase accuracy with proper decision support, reduce cost and infuse higher quality and better utilization, why would consumer perspective be left out of the equation? The patient’s access and health management, in my opinion is a fundamental component in achieving true Meaningful Use, and may drive quality beyond present measures designed by quality measurement developers–NCQA, NQF, AHRQ, etc.
It was great to read about your maturity model and all the posts that have followed. The HC system has been dysfunctional for many years, and there will be many struggles as the system matures. Someone asked me the other day what an HIE company does. The simple answer is that an HIE is able to exchange medical records between medical providers and patients. Preferably the exchange should be paperless. The governments goal is for the exchange of medical records electronically across the Nation Wide Health Information Network (NWHIN). This is where stage Five in your maturity model fits in. A few of the posters have compared HIE growth/adoption akin to “Boiling and Ocean.” My response would be: How do you eat an elephant? One bite at a time.