
The COVID-19 crisis is an acid test for the value of telehealth and remote medicine in patient-centered and community care. Our 2018 Telehealth report described the opportunities and regulatory environment telehealth contended in. Now, new exceptions and regulations by CMS, the Office for Civil Rights, and the FDA are easing access, deployment, and promoting the use of telehealth and remote care in the hopes of reducing strain on an over-taxed healthcare system. While these changes are being forced due to an episodic event, COVID-19, there is a strong likelihood that the changes will become systemic, forever changing how care is delivered.
Key takeaways
- Changes in federal and state regulations surrounding telehealth and remote care are expanding access to care for tens of millions of Americans.
- Many of these expansions, for example the changes in telehealth and Remote Patient Management billing for Medicare beneficiaries, will remain in place after the emergency is over.
- Language in the regulations expanding access beyond just COVID-19 treatment means a broad swath of patients will access and use some form of remote care in the next few months, and many more providers will be practicing using telemedicine.
- Fears and worries about standards of care, patient acceptance, and financial viability will be put directly and obviously to the test.
- The opportunities for remote medicine go far beyond video appointments. Creating a broad virtual health strategy that includes asynchronous elements, remote monitoring, and patient reporting is essential.
- While many small providers and systems will use consumer-level systems out of the need for convenience and speed, these are the most likely parts of the exceptions to be temporary. CIOs and systems need to prepare for what will remain usable after these changes are reversed.
2020 Reimbursement changes prior to coronavirus
In 2019 and 2020, multiple new CPT and HCPCS codes were publicized for remote and virtual care. CMS also removed the geographic and originating site requirements for telehealth appointments for Medicare Advantage patients, which represent nearly a third of the overall Medicare population. For the balance of Medicare beneficiaries, those requirements remained unchanged.
In response to the COVID-19 crisis, Congress passed the Corona Preparedness and Response Supplemental Appropriations Act on March 6th. Among other things, this allowed the secretary of HHS to open these telehealth opportunities to the full Medicare population. States have also acted, some through cost sharing waivers or parity mandates. CMS is encouraging commercial payers to expand coverage, offering waivers for payers to change their coverage options mid-year to expand telehealth access. Most major commercial payers now support telehealth services as well.
With patients reluctant to travel, this expansion of reimbursement can be a lifeline for practices struggling with the question of staying open versus staying safe. Major primary care and internal medicine practices in Massachusetts are now expecting to temporarily transition to entirely virtual and remote services. This has significant benefits for patients, both those with COVID-19 symptoms and those struggling with other health or wellness issues, as to date all federal announcements have been clear that coverage expansions are for all needed care, not just that related to COVID-19.
It’s likely that this expansion of services in Medicare would have happened eventually, but probably over several years. This is the single change most likely to stay in place after the end of the emergency.
Licensing and Provision of Care
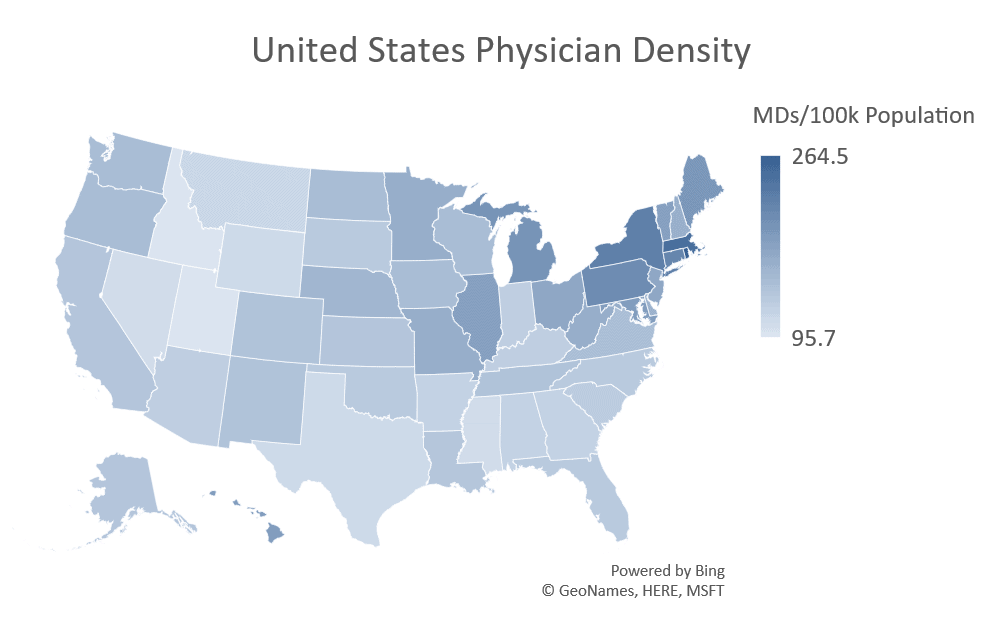
On March 13th, with authority granted by the Declaration of Emergency, CMS enacted waivers allowing providers with a license in good standing to provide care to Medicare beneficiaries anywhere in the United States. This was a landmark step, and essential to opening access to telehealth and virtual care nationwide. These changes allow for much truer load balancing across the national provider population. Without them, providers in low professional density states could easily become overwhelmed, even with the efficiencies or time savings offered by telehealth and remote care. Many, though not all, states have followed suit.
These limitations have been a significant obstacle to scaling telehealth and remote care deployments. The fact that direct telehealth does little by itself to save provider time is a major weakness of video appointments. Already, practices in Rhode Island, Washington, and Louisiana are reporting that the volume of virtual appointments that have been requested are overwhelming their providers. One Philadelphia system has reported a 10x growth in virtual appointments in a single week. As more patients are diverted to remote care and triage, these pressures will grow.
Systems need to be able to divert non-urgent appointments and requests away from overwhelmed providers and towards providers with more capacity. Expansions to the scope of practice for Advanced Practitioners (AP) will allow Nurse Practitioners, Physician’s Assistants, Advanced Practice Registered Nurses, and other APs to fully contribute as demand grows. While some states have resisted these expansions of licensure and practice scope, many others have adopted them even before COVID-19, and these changes are likely to last.
HIPAA and Enforcement Discretion
OCR, the office within HHS that monitors HIPAA privacy regulations, announced on Thursday, March 19th, that they would exercise “enforcement discretion” over use of non-HIPAA-compliant platforms for telehealth during the COVID-19 health emergency. The care that can be offered is explicitly not limited to COVID-19 care, as “a covered health care provider may provide… telehealth services in the exercise of their professional judgement to assess or treat any… medical condition.”
Not any video communication platform is acceptable under the revised standards. The technology must be “non-public facing,” meaning that live content or recordings cannot be accessible by other users during or after an encounter. Examples included “Facebook Live, Twitch, [and] TikTok.” Acceptable alternatives included Apple FaceTime, Facebook Messenger, Google Hangouts, and Skype.
For small practices and organizations that did not have a telehealth solution in place, this is a critical step to allowing patients to continue to receive care, albeit from a safe distance. In conjunction with policies that are greatly expanding what visits can be provided, reimbursement for many remote appointments are at the same rate as in-person visits . This will provide smaller practices a potential lifeline to critically needed cash flow to stay open.
In the long term, however, these solutions aren’t enough. Non-compliant platforms will pose dangerous privacy and liability risks when the exceptions are rescinded. These HIPAA exceptions are the least likely to be retained long-term. Options that have a HIPAA-compliant option but are still restricted to video appointments, such as Zoom Health, are still lacking in other areas. Remote primary care and care for chronically ill patients requires that monitoring equipment be in place, along with systems for receiving and recording their data.
Considerations for the Future
The loosening of these constraints allow health care providers and organizations to offer telehealth services while patients are restrained from or unwilling to travel. Hopefully, these changes to support telehealth alleviates the stress and burden on both providers that see the patients and the organizations that need to have patients seen to remain solvent. Telehealth through video chat is an excellent tool, but the best clinical results and the most effective relief comes from more than just remote appointments.
This article from a group of hospital MDs in Bergamo, Italy gives invaluable perspective from the center of a pandemic hotspot about what kinds of care changes are going to be most helpful as the number of sick increases. They include increasing outreach into the community and more effective and aggressive home care. That includes monitoring and care delivery within the home for mildly ill patients to reserve vital hospital resources for the most critical needs.
Video appointments will only be a part of the solution, and so can only be a part of a fully featured remote care platform. Announcements from the FDA that they are allowing vendors and users of FDA-cleared devices to modify those devices for home monitoring will help. It gives providers and the vendors supporting them much needed flexibility, and the ability to respond to needs quickly with the equipment they have on hand.
The longer the crisis persists, the more these exceptions will become a part of the new normal going forward. Some, like looser HIPAA requirements, will almost certainly be rescinded. Changes to reimbursement, to licensing, and even to scope of practice, represent the acceleration of changes that were already underway and thus likely to stick.
Even outside of these regulatory issues, however, we’re seeing a sea change in the use of telehealth. Patients have been open to remote care for years. What they haven’t been able to do is readily access it, especially with their primary care providers. However, COVID-19 has forced the issue and now it is providers reaching out to their patients suggesting a telehealth visit. Now that patients have been able to experience telehealth, will this be the preferred visit modality going forward?
Provider trust, organizational deployments, and the healthcare and business cases for it have been significant barriers but the current situation is breaking those down. As patients get used to telehealth and remote care and as providers and systems continue to make it part of their standard provision of care, it’s hard to envision going back to the status quo.
Telehealth and more broadly virtual care has been a technology on the cusp of “breaking out” for more than a decade now. COVID-19 is the spark that has lit the telehealth fire, a fire that will not be going out anytime soon.




0 Comments