Let’s take a quick look at the numbers. (For sake of simplicity, this post will look at physician reimbursement.)
For adopting and meaningfully using a certified EHR a physician may be reimbursed between $44K (Medicare) to $65K (Medicaid). This will not be a lump sum payment, but is parsed out over 5 years as the physician continues to demonstrate meaningful use of an EHR. Important points here, the physician pays up-front costs (sunk capital) and is reimbursed over time if he/she can demonstrate meaningful use and the solution adopted is “certified.”
As the latest Wal-Mart, Dell and eClincalWorks partnership shows, vendors looking to sell into this market opportunity are pricing their solutions at or near reimbursement levels, e.g., $25K year one and $4-6.5K for follow-on years in the Wal-Mart offering.
According to athenahealth CEO, Jonathan Bush, their customer, a physician, grosses $400k/yr.
Virtually every report we have seen and physicians we have spoken to who use an EMR/EHR today, readily admit that the upfont pain of implementation, training and becoming adept at using the solution was significant. The significance is most often felt in an average 30% productivity hit for the first 6 months that is compensated through longer hours or seeing less patients. The proactice does not return to pre-implementation state of operation till a year after go-live.
Combining the above and keeping calculations simple: (Note: we’ll assume productivity returns to previous state within first year and use a sliding scale for productivity hit in year one of, first 6 months 30% hit, second 3 months, 20% and and last 3 months 10%)
Year One Cost: ($25K) for EHR purchase + (0.30($400K/2) + .2($400K/4) + .1($400K/4)) = ($115K)
Year One Reimbursement: $25K (more generous Medicaid)
Total Cost to Physician: ($115K) + $25K = ($90K)
After Year One, the physician is already down $90K. Assuming practice returns to normal operations/productivity in years 2-5 and the physician is successful in getting full reimbursement from Medicaid, at the end of five years, that physician is still down $50K. Depending on how much business the physician derives from Medicaid, it will take many more years of avoiding the “stick,” the sliding decrease of Medicaid payments, before a physician recoups this initial, year one loss.
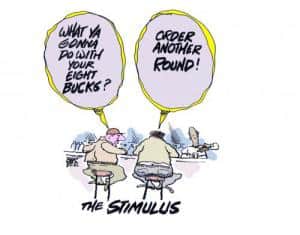
Bottom-line: Adopting an EHR to tap that $19B dollar Stimulus package does not make economic sense for the average physician.
Solving the Physician Adoption Problem
To drive EHR adoption we will need three things:
1) Low “meaningful use” thresholds to ease the pain that a physician has to go through to demonstrate that indeed they are meaningfully using an EHR. As a starting pointing, let’s target electronic exchange of labs, meds and vitals (including allergies) for care coordination combined with eRx. That should address care coordination, quality and eRx outlined in HITECH Act.
2) Very simple certification process for HIT. Do not burden the system with complex certification processes, ala CCHIT. Don’t get me wrong, CCHIT has done some good things in the past, but to apply CCHIT certification for “certified EHR” will create far too complex and onerous a process for truly new and innovation approaches to provide solutions that assist physicians in meeting meaningful use criteria.
3) Leverage the consumer to create an additional forcing function to drive physician adoption as reimbursement under the HITECH Act is insufficient. Getting the consumer engaged may prove challenging, but engage we must for at the end of the day, the value in a physician adopting and using an EHR must return to the end consumer/taxpayer as they are the one footing the bill.
Over the next few years we, as a nation will be extremely challenged to drive true healthcare reform, healthcare reform as President Obama stated that is “evidence-based.” A common refrain in the manufacturing industry is: “You can not improve what you do not measure.” Today, our healthcare system has absolutely no systematic way of measuring its performance. It truly is a travesty. Healthcare IT can, if effectively deployed and used, can play a critical role in collecting those measurements that we can begin to use to conduct true, evidence-based reform.
We need to articulate to the Joe the Plumbers of this country, what HIT adoption and use means to them. To date, the healthcare industry and government has done an extremely poor job of helping Joe understand that value. Without his/her support, no amount of money thrown at this problem will suffice.




What R the chances U think I’ll get reimbursed for my investment in an EMR/PMS in 2006?
Great post and analysis.
I think that you have pointed out, yet again, the great challenges facing many HIT solutions – how do you encourage adoption if a solution that does not fundamentally improve revenues or reduce costs in a way that offsets the upfront investment.
Without ROI, why should a MD or clinic change?
John – At the end of the post you state “Today, our healthcare system has absolutely no systematic way of measuring its performance.”
Do you think that these measurements should be purely clinical in nature (outcomes, chronic care mangement, etc.), or that operational measures also should be part of this analysis/national imperative (patient wait times, lab results delivery turnaround, etc.)?
It seems to me that the way you make this work for the Joe’s out there is to describe how HIT will improve their interactions with the healthcare system.
John, I’ve said it once, but it bears saying again, all this increased HIT activity at the federal level has brought out the best of your inner-blogger. Continue to enjoy reading your analyses.
Couple of great questions I’ll try to answer:
Shelley,
Nothing is clear at this point but looking at past actions of HHS tells us that those who have an EMR in place today that meets the criteria for “certified” (CCHIT? I don’t know) and are actively using the EMR in a “meaningful” way will be reimbursed. Unlikely to get one big lump sum for past years’ use, but can begin to collect in Year One of disbursement.
NL,
For us “Joe the Plumbers” believe the vast majority will want to see evidence that the doctor’s use of an EMR in some way makes their life easier. Seriously doubt that clinical measures are going to do. Looking at what is popular over at KP is instructive as to what consumers will find value in:
Rapid, electronic delivery of lab results,
Ability to request script refills online, as well as have med list to share,
Ability to make appts & request referrals online,
eVisits
These are the key services that KP has found average consumers aggressively adopting and using as it makes it easier for the consumer to interface with the healthcare system.
For those with a chronic condition or assisting a loved one with such, digital records for care coordination become more critical.
Thanks or the great comments.
John
I really love your analysis of the financial costs and benefits of a physician voluntarily purchasing and widely adopting an EMR system under the HITECH Act.
But I don’t think it goes far enough to add in all the variables and to properly set the context for the physician’s decision-making process. Even self-interest, you might agree, can be stretched to enlightened self-interest, if one has all the facts.
EMR systems are not launched in a vacuum.
First, their purchase and wide-scale adoption can be voluntary—or they can be de jure mandated or de facto mandated (the last of these means that they are voluntary in name only, since you won’t get paid or at least you won’t get paid as much if you don’t really adopt and use one). I think most US physicians, regrettably, fall into this very last category. I say regrettably, because I spent a lot of my time and a lot of the AMA’s money giving regional talks to the physicians regarding their use of technology of all sorts to improve quality, increase productivity, reduce tangible and intangible costs, and, perhaps most importantly for them, reduce malpractice suit and liability exposure. If I had one debate, I had a thousand, with really smart physicians about the value of a clean, crisp, legible medical record, one with time and date stamps, and warning flags, and the like, when it came time to avoid suit or at least avoid losing one–or at least paying a multi-million dollar judgment or settlement over your insurance coverage. They all believed that the clear record would sink them, not save them, and even joked about that widely held point of view being the reason they scribbled their entries into the record—so they could say that they meant something different when the case came to trial. They couldn’t have been more wrong on all counts. And, believe it or not, I actually convinced a few of them to look at it my way.
Second, your analysis does not take into account the many obvious benefits to patients, families, and employers, as well as payers—all of whom the physician should care something about, if for no other reason than it makes good bedside manners and leads to a full and satisfying practice—because if the patient is dissatisfied, everyone is dissatisfied. Such benefits include the avoidance of harm (death or disability), suffering (and stress), and tangible and intangible costs (paid indirectly, for example, by one’s employer; or paid directly as out-of-pocket costs). It also speeds up the process and lets everyone sleep better at night, since errors of both commission and omission are reduced by a sound EMR system. (Of course, not every EMR system out there is a sound one, but that is what we want some reasonable form of certification to help us guard against.)
Third, you show only loss of productivity, not the many improvements to productivity, quality, coordination, and follow-through, to name but a few of the more obvious benefits, which can flow from a good EMR system, especially one that has decision-support and medical-knowledge-processing systems layered on top of it. Such layering, of course, would not be possible, unless the basic EMR system was already in place. I cite, for example, the case of Summit Technology, the worldwide inventor of the laser-eye-surgery industry, where I was personally a major player for more than a dozen years, and I therefore have first-hand knowledge, not just book-learning-knowledge, to fall back on. My Summit colleagues and I took a nearly bankrupt company and turned it around by proving to physicians, nurses, and technicians (but especially physicians) that we could boost their personal productivity dramatically by automating many of their diagnostic and healthcare-services functions. They were happy with the outcome. Patients were happy with the outcome because of dramatically increased access and lower aggregate and net costs. And my colleagues and I were happy with the outcome—both because of the difference we hade made in all stakeholders’ lives, especially patients’ and providers’ lives, but also because of the $ Billion sum that we received when we sold the company to Nestle.
Finally, for now, fourth, you look at the issue from the perspective of a person who looks a gift-horse in the mouth. For the benefit of their patients and their own staffs (and themselves, of course) most physicians should have purchased and widely adopted a good EMR system many years ago! It would have made life better and simpler for all stakeholders. Instead, being the small business men and women that they are, they have wrongfully held out for two things: first, an ideal system, which will never be invented; and second, a full-repayment from the federal government for something that is an investment in their own productivity, profitability, and difference-making. I would say that the cup is at least a third full, not two-thirds empty. The enlightened government under President Obama is willing to help them do what they should do—and should want to do—for themselves and for their various stakeholders/constituencies. The amount of funding, while modest, by a strictly financial measure, is at least a good “hand-up,” when Medicare would be perfectly within fair bounds to insist on some measure of modern automation without any direct compensation.
I want to apologize for being a bit long-winded in my earlier comments. I think you can get the point, though, that I am passionate about getting, particularly physicians, who hold so much power under our current healthcare delivery system, to “do the right thing,” as one rising tide lifts all boats. Physicians should lead the way in creating, and continuously improving, a higher-quality, more-accessible, more-robust, more-coordinated, more-outcomes-oriented, more-patient-centric, and more-cost-effective healthcare delivery system for the nation they love and for all of its residents, something that can be held up as a model for the world to replicate. The time for unenlightened-self-interest and corporate-greed has closed. In other words, let’s all pitch in, put our backs into the oar, and steer a straight course for a Renaissance in American healthcare. It will help make a better world for us all.
Best,
John