In this Chilcast episode, John Moore sits down with Deepak Sadagopan, COO of Population Health at Providence and CEO of the Providence Medicare ACO, Health Connect Partners, to discuss the strategic imperatives for healthcare executives navigating the transition to value-based care (VBC).
The Promise of Clinical Data Sharing
About a month ago, I ruffled a few feathers. The brief post highlighting the increasing interest...
eCQMs: Beginning of a Long and Rocky Road
A New Necessity Payment-based upon quality measurement is at the center of a wide range of efforts...
The Waning Influence of ONC
Market Challenges Many are beginning to question ONC’s role in the further promotion of EHR...
Struggling to Understand or Data Does Not Equal Empowerment
Recently upon leaving my doctor's office I was presented with a print-out of my visit summary....
Reading the Tea Leaves: CMS to Release MU Rules this Month
The healthcare IT (HIT) industry waits with baited breath for the release of preliminary...
Meaningful Use Draft is Tough to Swallow
Today, the Meaningful Use (MU) workgroup of ONC's HIT Policy Committee presented its...
Usability & Adoption of EHRs
Policy makers keep wondering why physicians do not readily adopt EMR/EHR software. Under ONC's...
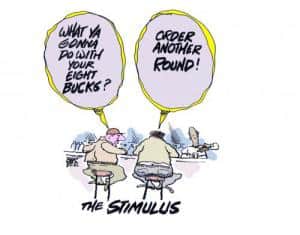
The HITECH Challenge: Is $19B Enough to Drive HIT Adoption
With the HITECH Act passed and the Dept. of HHS feverishly working to draft a clear definition of...