As I sat in the Reading (Penn.) Health System ER late Friday night, I had a lot of time to reflect on the research I have been doing lately on care coordination. In particular, I pondered how what I have heard and seen among many demos the past several months compared to the state of care coordination my mother had received earlier in the day and was receiving at that very moment – all this amid the constant cacophony of chirps and beeps emitted from the controlled chaos in the ER that night.
The events that brought my mother to the ER had occurred several hours earlier. Right before 5 p.m., my father called to say my mother had been experiencing severe nausea with vomiting and diarrhea since earlier that afternoon. In the past hour, she had been unable to even keep down electrolyte-infused water.
For most people, the common recourse is to take a multi-symptom OTC drug such as Loperamide, lie down, and try to sleep as this stomach bug worked its way through their system. But my mother has a chronic kidney disease with a severely impaired renal clearance rate (RCF), so this simply was not an option. Severe dehydration risked spiking her already elevated protein levels and possibly causing further kidney damage, which she could ill afford.
Before calling me, though, my father had called my mother’s nephrologist at Penn Medicine. He had already left for the day, but my father reached him on his personal cell phone number. The nephrologist had given this information to my mother several months ago, along with his home number and personal email address. This certainly was not a standing practice or policy for Penn Medicine, nor was it something that other physicians at Penn had done for my mother over the past several years. It was simply due his own sense of professionalism and obligation in the doctor-patient relationship.
The nephrologist said my mother needed to be seen immediately at the nearest ER, started on an IV to rehydrate her, and given additional medications to stop her vomiting and diarrhea as necessary. He also told my father to provide his contact information as soon as my mother arrived at the ER; the nephrologist wanted to further explain the situation and speak to the attending physician, regardless of the hour.
I drove to Reading, picked up my mother, and went to the ER. After we went through security, we were met by a long line to even submit her name. Unfortunately, Reading has one of the highest rates of poverty among U.S. cities, and this manifests itself in a high rate of uninsured people who often end up in the ER. On a busier-than-normal Friday night, the estimated weight time exceeded 3 hours.
I tried explaining my mother’s situation to the admissions desk, as well as her physician’s instructions to be seen immediately. However, since my mother was not experiencing chest pains or severe trauma, she was told to wait. At this point, I called my mother’s nephrologist, who demanded to speak with the admission desk staff. While all this was occurring, my mother proceeded threw up in a bag she had brought with her.
That, along with the nephrologist’s conversation with an attending nurse at the front desk, thankfully got my mother processed nearly immediately. She had her basic information verified and her vitals taken. Then she was moved to a transfer bed close to a restroom, where staffed started an IV, gave her anti-diarrhea and anti-nausea medications, and took her blood to start lab work.
Within a few hours, my mother was in a formal ER bed and we were finally able to speak with an attending overnight ER physician (an internist). He explained the results of the blood work, reviewed my mother’s recent medical history, and discussed the next steps, which included admitting her to ensure she only had a stomach bug and not a bout of diverticulitis or c. diff. The attending ER physician had also heard from my mother’s nephrologist, who wanted to discuss her case before she was admitted or given any additional further medical treatment. He said they talked for nearly 25 minutes. I was really surprised to hear that my mother’s nephrologist had been willing to discuss her case with this attending physician at 11 p.m. on a Friday night.
Care Coordination & Health IT shortcomings
While technology, especially mobile phones, played a vital role in coordinating care for my mother Friday evening and ensuring she got the proper care she needed in a timely manner, almost none of it came from health IT solutions. Even medication reconciliation had been largely facilitated by a copy of my mother’s medication list from her MyPennMedicine record (an Epic MyChart application) that I printed before we went to the ER. I also had brought along her pills and ledger notebook where she notates what she takes, just in case the printed list was missing something.
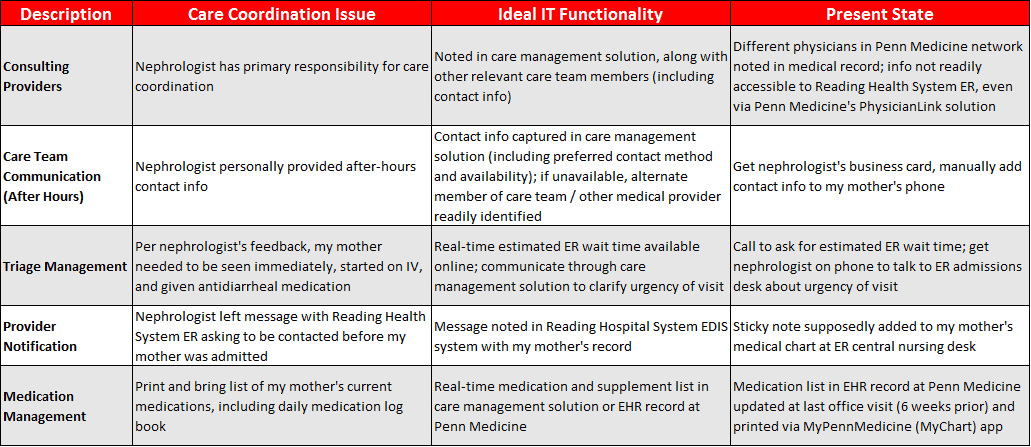
The glaringly evident limitations of the health IT solutions I witnessed Friday evening have been discussed ad nauseum, including the lack of interoperability of EHR systems and the inability of patients to access and easily share their medical history as necessary. (See the Table below.)
What really struck me before I left the hospital at close to 1 a.m. was that, despite all of the talk about the need to better coordinate care through the use of various care teams and longitudinal care plans, it really was the dogged persistence and professionalism beyond any normal expectation from my mother’s nephrologist that enabled her to get the care she needed. For that I was incredibly grateful — but also a bit dismayed, as massive investments in health IT the past several years did so little to coordinate the care my mother needed that evening.




0 Comments