Prior Authorization is often viewed as the poster child for throwing the Quadruple Aim off balance...
Driving Policy Without Healthcare Organizations: A Fool’s Errand
Healthcare in the United States faces many problems, but one of the bigger ones is bringing the right stakeholders to the table when it’s time to try to solve a problem. Often, the empty chair should be occupied by an individual – the overwhelmed patient, the uncompensated caregiver, the burned-out doctor or nurse. Rarely is an institution not represented.
Vendors Enabling the ACO: New Class of Vendors Matures
Successfully enabling an Accountable Care Organization is extremely challenging: There isn’t one standard ACO model; there isn’t one single ACO national policy; there isn’t one specific map to follow to build an ACO nor measure its success. There are few if any best practices readily available for healthcare organizations to adopt and make a successful transition to value-based care (VBC) within an ACO model. This has created a strong market need for high-service solution vendors (“ACO Enablers”) that can guide healthcare organizations (HCOs) on the ACO path.
Navigating Open Enrollment – Or, Why Informed Choices in Healthcare Are Nearly Impossible
Like many Americans, I have been covered by employer-sponsored health plans for the entirety of my...
RCM Meets PHM
It won't happen in 2017 or 2018, but the argument can be made that PHM will likely include some...
What You Can Control and What You Cannot
I prepared last Thursday’s webinar with no idea how the election would turn out. As it...
Changing of the Guard: Implications to Health IT Market
After a brutal election cycle, we are now on the other-side. The Republicans have taken control of...
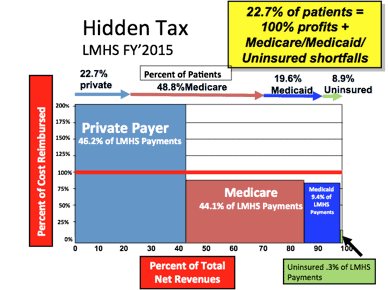
Value Based Health: No Success without Value-Based Technology Strategies
A September 16 2016 Bloomberg report once again provides the bad news for the US healthcare...
Analytics – An Integral Part of Care Management Success
Last week, I attended the 3rd Health Analytics Summit (HAS). This was my first time attending an...