Key Takeaways
- Interoperability is an imperative that HIT business models simply must accommodate. Red flag warning to all healthcare IT vendors large and small—plan to data share to enable a connected ecosystem, or risk the erosion of market share and future demise.
- Among traditional EHR vendors, Cerner is market-leading with their interoperability strategy. As such, they are being rewarded by the market with an exponential increase in sales, including three non-Cerner EHR clients for HealtheIntent so far, and a rich sales pipeline for their EHR-agnostic cloud-based HealtheIntent population health platform.
- While there were many encouraging examples of operational improvements highlighted by ACO clients throughout the conference sessions, there was a noticeable absence of any emphasis on proven ROI at this stage of the HealtheIntent (PHM) product lifecycle.
- Simply stated, Care Management technology across the industry could use an overhaul.
- No one is taking a pause in their HIT investments as a result of the election.
- Standing ovation for Cerner CEO Neal Patterson, for his surprise contribution to the keynote address!
- Neal Patterson, for his surprise contribution to the keynote address!
More on the Interoperability Theme
Integration as a dependency to long term HIT viability cannot be overemphasized. We have reached the tipping point—to be vendor agnostic or not, participate in open data sharing or not, be a data integrator or not. Vote for interoperability. We learned of vivid examples of vendor solutions that chose not to fully integrate and consequently lost all previously strong adoption. Provider workflow and efficiency crumbles when they are forced to work across multiple interfaces.
As a sign of market evolution, we witnessed the success of empowered providers exerting influence over vendors in a push for greater interoperability. Let this serve as a call to providers to expect interoperability from your technology vendors as the optimal approach. Don’t assume you need to “go it alone.” We talked with providers who attempted to build their own code to integrate disparate systems, only to eventually give up after years of sunk cost and lost productivity. On the flip side, only when providers also share their data can the ecosystem function as truly open and optimized for value.
Cerner has certainly evolved their open platform strategy embarked upon several years ago when they partnered with then Certify Data Systems for HIE, and more recently being a founding member of Commonwell Health Alliance. In Q3 2016, Cerner officially opened HealtheIntent PHM and Millenium EHR to third party developers via the brand “code” – a development environment that includes a multitude of APIs. Cerner has also completed custom coded integration with competitor eClinicalWorks (eCW) for even more seamless interoperability of HealtheIntent modules in an eCW clinician’s workflow, an indicator of how client requirements are driving transformational vendor relationships in healthcare.
Cerner’s multi-pronged growth strategy consists not only of serving up an open ecosystem, but also includes planned expansion and refinement of HealtheIntent with new network functionality to better enable value-based arrangements. New modules targeted for GA in 2017 include referral, contract, and network management, allowing a CIN or ACO to project their success in launching a risk-based arrangement, evaluating not just standard population clinical risk and opportunities, but also layering in network coverage determinations by geography.
Care Management: Certainly Adequate, But We Need To Do Better
We liked Cerner’s “value-based” pricing strategy for the HealtheCare care management module of the HealtheIntent platform. The user is exposed to the entire population registry and able to identify care management targets by filtering against varying criteria (diagnosis, open care gaps, risk score). However, software cost is accrued only for the volume of the population actually moved into Care Management programs, where the value realization potential exists.
HealtheCare sales have increased at a steady rate year over year since 2015 GA, as providers need a solution for Care Management that is more advanced than home-grown spreadsheets, SharePoint sites, or paper. HealtheCare delivers on those basic expectations, but we found the user interface fed by the underlying architecture to be dated. To be clear, it wasn’t that HealtheCare is missing any expected functionality; it was that it didn’t include anything exceptionally innovative.
This is an industry-wide issue wherein most of the Care Management solutions we have reviewed for our upcoming Market Trends Report all have a similar look and feel – a glorified spreadsheet with pick-lists. It’s time for an entirely new construct in Care Management technology, time to rethink Care Management as the community engagement tool that it is, to create a contemporary platform to truly engage all stakeholders including consumers, caregivers, and community.
A Poignant Reminder How Interoperability Improves the Consumer Experience
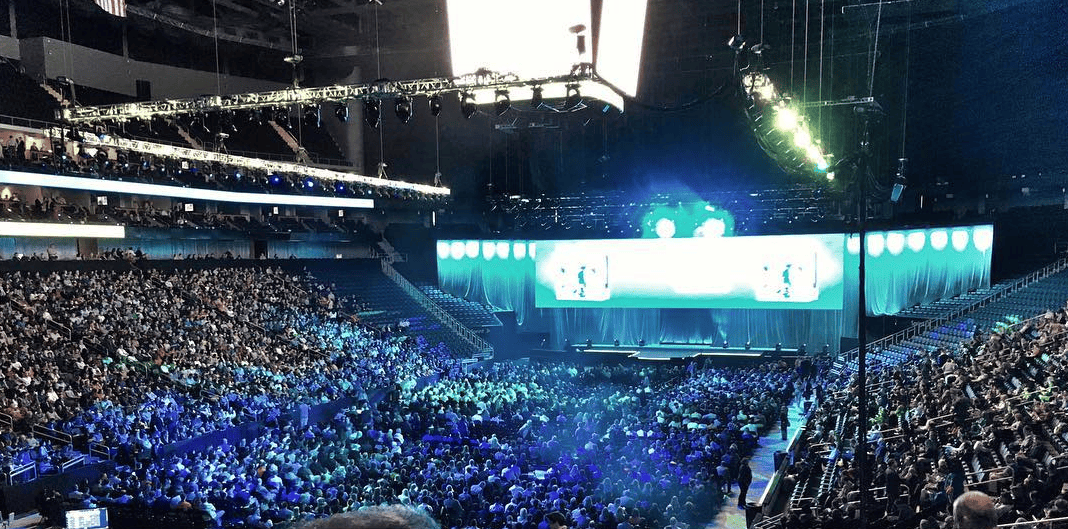
Why are we even doing all of this grueling work to revolutionize healthcare? The keynote address brought it all home for the 15,000 attendees in the Kansas City Sprint Center. Caring. Consumer experience.
I witnessed hands down one of my most moving moments in 25 years in healthcare. First, Geisinger CEO Dr. David Feinberg walked us through a systematic approach for elevating the consumer experience. It simply couldn’t get more inspirational, then Cerner CEO Neal Patterson took the stage and delivered a surprise address despite–and because of–undergoing extensive treatment throughout much of 2016 for soft tissue cancer. His gift is to now turn his own personal experience, profound and troubling as it was, into a drive for further system-wide improvement.
It doesn’t get any better than that, Neal.
Kindness and caring is not about reducing wait times; it’s about eliminating them. It’s about using data to anticipate a consumer’s health issues. It’s about ensuring consumers can readily participate in their care and access their consolidated medical record and care plan inclusive of input from all care providers on their team, absent annoying and exhausting technology or data sharing impediments.
As Neal concluded his address, “We’ve done much, but there is so much more to do.”




0 Comments