I prepared last Thursday’s webinar with no idea how the election would turn out. As it happens, few – if any – in the pundit class knew either. And while there are many changes likely coming to healthcare as a result of the election (as we discussed in last week’s post), no one can predict what they will be with absolute certainty.
However, there are things providers can do no matter what comes out of Washington. One of which was the subject of my True Continuous Costing webinar (links to recording and slides). What we do know, with a great deal of certainty, is that the stifling cost of healthcare in the USA has to be reduced. For most people in our country, the major issue they face with healthcare is not the quality but the price they are expected to pay. Unless something is done immediately, the cost of providing care will go up even further and these increases in costs will simply be passed on to patients, one way or another.
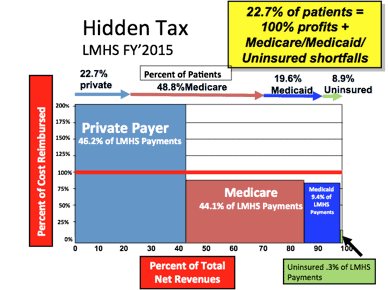
The good news, as we demonstrated in the webinar and in the report, providers have many tools at their disposal to reduce their costs. These cost savings can be passed on to patients. Why this is not being done universally throughout healthcare is quite the mystery. To illustrate the problem I want to thank the Lee Memorial Health System of SW Florida for the following chart:
The red line is break even. As you can see, private insurance provides all the profits at Lee Memorial and covers the shortfall from Medicare, Medicaid, and uninsured patients. As long as nothing changes Lee Memorial will continue to be one of the great county-owned and operated healthcare systems – fully self-sustaining and not requiring tax payers to pony up money to make up for operating losses. But the risks are obvious.
Any shift in the percentage of private payers or private payer payment levels downward is a serious threat and expecting Medicare or Medicaid payment levels to go up to cover this revenue loss is risky in the extreme. Also, getting the uninsured insured helps some, but the better trend would be to get them into private vs. government paid healthcare insurance.
But there are three likely changes to the financial picture. First, the mix could, and likely will, shift to more Medicare. Second, CMS wants to cut Medicare payment amounts. Some of this is cloaked in “quality” and “savings” schemes, but the bottom line is CMS is about cutting payments. Third, it is likely that under the new administration Medicaid will migrate to block grants to States, creating further challenges, especially for those who have received subsidies to purchase health insurance leading to more uninsured. Fourth, keeping that red line in check in real dollars is a huge challenge.
In the webinar we talked about how to actually move that red line down in real dollars. In fact, that is the entire scope of my research – how to lower the cost of care using data, technology and proven best practices.
I will not rehash the webinar and the report here, other than to say there are providers doing it, and it is making healthcare more affordable. It takes a change in attitude and culture, but this chart gives evidence in black and white for the motivation to make those changes.




Update: I want to clarify one thing. I am not certain that Medicaid block grants will definitely mean more uninsured. In fact, nothing is certain. However, I am suggesting that expecting any future Medicaid reimbursement scheme to move towards par with private insurance is unreasonable.
The bottom line remains the same: the one area where providers have tremendous unused leverage is over their costs of providing care. Since the webinar, more data points on success in reducing the cost of are trickling in. I am delighted to take calls or emails to discuss this on-going work.