
There is no question that indeed, the HITECH Act has achieved one of its primary objectives – foster the adoption, via incentives, of certified EHR technology (CEHRT). This is truly a good thing, for only by digitizing health data can we then move on to further public health policy goals of beginning to understand what actually contributes to health and well-being (comparative effectiveness), and also move towards a model of personalized medicine and true patient engagement.
But at what point does the government’s role in fostering adoption of CERT end and market forces begin?
A Little History:
To foster adoption of CEHRT but also ensure that tax payers (after all we’re the ones footing the bill for these incentives) get value from said adoption, ONC pulled together a number of workgroups to define “meaningful use” requirements that physicians and hospitals would need to demonstrate to get their incentive payments. This was broken up into three “Stages” with each stage building upon the previous.
The first stage of “meaningful use” requirements were pretty simple as the plan was to just get the medical establishment to begin adopting CEHRT and familiarize them with usage of this tech. The incentive payments were also front-end loaded (receive more for meeting stage one than subsequent later stages) so low and behold, we saw strong adoption and attestation for stage one. Hip, hip hooray were the cheers heard at the Hubert Humphrey building in DC.
Where We Are Today:
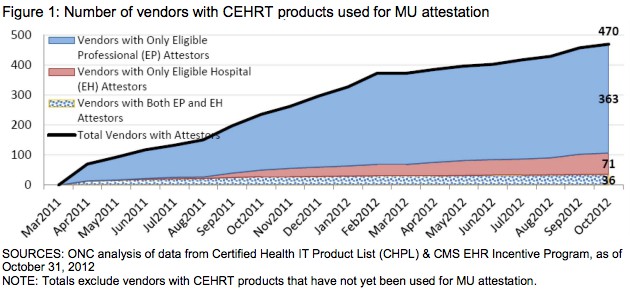
But that low barrier to stage one adoption created a false market for EHR technology. There is now a plethora of EHR vendors, especially on ambulatory side that frankly should have never made it this far.
Meaningful use stage two requirements for certification are a significant hurdle for many of these EHR vendors who simply do not have the resources, nor technical chops to meet them. Sadly, a lot of ambulatory practices will suffer as a result. This in large part led to the proposed rule released this week by CMS to allow providers to postpone attesting with stage 2 CEHRT this year and allow them to attest with 2011 CEHRT. It is CMS’s hope that this delay will provide EHR vendors the time to get their act together and be certified for stage two as well as provide sufficient time for providers to adopt these updated systems to attest.
Time to Step Out of Way and Let Market Takeover:
But as often happens with government initiatives, initial policy to foster adoption of a given technology can have unintended consequences no matter how well meaning the original intent may be.
During my stint at MIT my research focus was diffusion of technology into regulated markets. At the time I was looking at the environmental market and what both the Clean Air Act and Clean Water Act did to foster technology adoption. What my research found was that the policies instituted by these Acts led to rapid adoption of technology to meet specific guidelines and subsequently contributed to a cleaner environment. However, these policies also led to a complete stalling of innovation as the policies were too prescriptive. Innovation did not return to these markets until policies had changed allowing market forces to dictate compliance. In the case of the Clean Air Act, it was the creation of a market for trading of COx, SOx and NOx emissions.
We are beginning to see something similar play-out in the HIT market. Stage one got the adoption ball rolling for EHRs. Again, this is a great victory for federal policy and public health. But we are now at a point where federal policy needs to take a back seat to market forces. The market itself will separate the winners from the losers.
The move to value-based reimbursement (VBR) will force healthcare organizations of all sizes to adopt some aspect of population health management. Interoperability, the big sore point today is not so much a technology issue as it is a market issue – and population health management is impossible without interoperability. While I know that the new ONC director, Karen DeSalvo is well-meaning in her intentions, interoperability is something that market needs to sort out, not ONC. My fear is that by letting ONC/CMS define interoperability, we will be left with highly prescriptive definitions and not innovative models, which this market desperately needs.
I applaud the hard work and efforts of all the public servants of HHS and volunteers who have worked tirelessly to get us to the point of where we are today. However, it is now time for them to refocus their efforts elsewhere. Maybe a good place to start is to assist all those ambulatory practices that have adopted a CEHRT under stage one to assist them in the transition to a more viable and stable EHR vendor for the long-term. Then again, maybe this is just an issue of caveat emptor.




I agree with you in so many ways. Innovation is lacking because the government is still prescribing what should happen. I wrote an article with a somewhat similar message where I called for HHS to “blow up meaningful use”: https://www.linkedin.com/today/post/article/20140515213807-6749519-my-plan-to-blow-up-meaningful-use-and-make-it-useful?trk=mp-author-card
I do disagree with you on letting the organizations handle interoperability. I don’t think they’ll do it if there’s not some external incentive and value based reimbursement won’t be enough.
Excellent and insightful post. MU has diverted attention and resources away from innovation that can truly change outcomes. Smaller firms (read innovators) have to spend precious resources figuring out how to more easily interface with EMRs than advancing their life saving technology. Inpatient EMR firms, if they so choose, can now dictate to hospitals what tech to use. When this happens – and it occasionally does – outcomes take a back seat to business interest.
I believe that MU Stage One was laudable and the only thing I would have changed is telling vendors that out-of-the-box, their solution needed to be interoperable with a set of open APIs. Now we must live with data silos of some 400+ different EHR solutions that have been adopted – it will take some time and a lot of $$$ to work that one out. Beyond Stage 1 it is highly questionable as to just how effective the more prescriptive requirements really are or are we causing more harm (as you point out) than good.