 Chilmark has not been a big fan of the National Health Information Network (NHIN) concept. It was, and in large part still is, a top heavy federal government effort to create a nationwide infrastructure to facilitate the exchange of clinical information. A high, lofty and admirable goal, but one that is far too in front of where the market is today. The NHIN is like putting in an interstate highway system (something that did not happen until Eisenhower came to office) when we are still traveling by horse and buggy. Chilmark has argued for a more measured approach beginning locally via HIEs established by IDNs (our favorite as there is a clear and compelling business case) and RHIOs in regions where competitors willingly chose not to compete on data, rather seeing value in sharing data.
Chilmark has not been a big fan of the National Health Information Network (NHIN) concept. It was, and in large part still is, a top heavy federal government effort to create a nationwide infrastructure to facilitate the exchange of clinical information. A high, lofty and admirable goal, but one that is far too in front of where the market is today. The NHIN is like putting in an interstate highway system (something that did not happen until Eisenhower came to office) when we are still traveling by horse and buggy. Chilmark has argued for a more measured approach beginning locally via HIEs established by IDNs (our favorite as there is a clear and compelling business case) and RHIOs in regions where competitors willingly chose not to compete on data, rather seeing value in sharing data.
But what might happen if the folks in DC stopped talking about the NHIN as some uber-Health Exchange, but instead positioned it as a consumer-focused platform?
That is basically what happened yesterday at the ITdotHealth event where the new federal CTO, Aneesh Chopra and new HHS CTO Todd Park presented their conceptual idea to a pretty select group who had gathered together to discuss the idea of platforms in HIT to support discrete, substitutable, modular apps. (John Halamka gave a nice write-up of the event in which he participated on the first day). Chopra and Park were seeking to float this idea among the movers and shakers of new models for HIT, gauge the interest and ultimately solicit support for the concept.
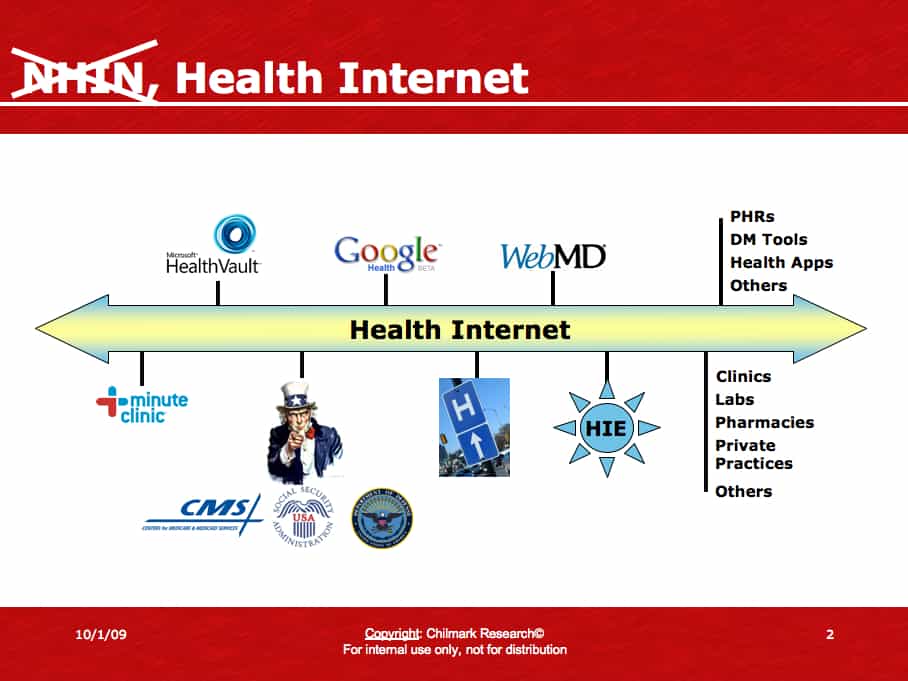
In somewhat of a re-branding exercise. Chopra and Park are proposing that the NHIN now be viewed not so much as solely a clinician to clinician care coordination exchange platform but rather one that also will focus on the consumer, creating a secure Health Internet to facilitate consumer access to and ultimately control of their personal health information (PHI). The basic NHIN, let’s now refer to it the Health Internet, is still composed of the same technology stack: platform independent, open source, freely available with published standards, etc. that support an independent software vendor’s (ISV) ability to build apps upon the Health Internet stack for consumer consumption (e.g., health & wellness services, PHRs, etc.). In June, we attended the NHIN CONNECT conference and our write-up provides a few more specifics on the Health Internet.
At the ITdotHealth event many of the participants (Google Health, HealthVault, MinuteClinic, etc.) stated that they “are in” and are willing to work with the feds to insure that their respective platforms/services will be able to readily connect to and exchange PHI upon a consumer’s request over the Health Internet. Even EMR giant Cerner voted tentative support for the idea if the Health Internet would assist them in helping their customers (clinicians, clinics, hospitals) meet some of the forthcoming meaningful use criteria that is now being formulated by CMS – Chopra at the June CONNECT event and Park at this one basically inferred that providing the capability for an EHR to connect to the Health Internet would address some aspects of meaningful use.
Chopra also stated that he has the support of numerous federal agencies (DoD, CMS, and other agencies) who are now working together with HHS to define how the Health Internet might serve their respective constituents. These agencies have not yet formally committed to allowing PHI to migrate to the Health Internet, but today are addressing the critical process issues of consumer access, control, and consent as it pertains to on-ramping PHI to the Health Internet. Chilmark believes that these issues will be resolved within the year. When that happens, we can expect some pretty significant movement of PHI across the Health Internet. For example, the DoD alone has nearly 4M active duty members (multiply that by 2.2 for dependents and the number skyrockets to over 8M) whose PHI may begin to flow on the Health Internet.
And it is not just Google Health, HealthVault or others that may be beneficiaries of the Health Internet. In speaking with a representative of the VA (yes, VA is a supporter as well) he related that this will allow veterans an opportunity to choose the best services out there in the market to assist them in managing their health. No longer will the VA have to try and create such apps themselves, or find partners to create the apps to sit on top of the VA PHR HealtheVet. Instead, the VA can simply direct a veteran to the Health Internet where such services will reside and instruct a vet as to how to access those services.
This is exactly what Chopra and Park envision with Chopra adamantly stating at the beginning of his talk that they seek, through the Health Internet, the creation of a fertile environment where innovation can flourish and ultimately consumers will benefit.
Finally, HHS & the Feds are Talking About the Consumer
Chilmark has been quite disheartened as of late with the lack of attention paid to the consumer, the citizen who is footing the bill to get doctors and hospitals wired. We chided the HIT Policy workgroup for HIEs for their complete lack of acknowledging the consumer’s role and ownership of PHI. We came back from DC recently disillusioned at the nearly myopic focus of ONC on clinicians. Chilmark is concerned that the $44k allotted to a physician to adopt an EHR is not enough, another forcing function is required and what better forcing function than the citizen, the customer of the physician to drive adoption of EHRs.
Low and behold others at HHS and elsewhere had similar feelings and are now moving aggressively forward with a concept that directly addresses the consumer. Hallelujah!
The Plan:
At the ITdotHealth meeting, Park and Chopra stated that if interest is high (sure seemed to be at this meeting), they wanted to take that feedback back to DC and work with the federal team to start laying the groundwork to get started ASAP. Hypothesized goals and objectives include:
The federal team will begin by working with industry stakeholders (PHR providers, EMR providers, services, hospitals, fed agencies, etc.) to identify the gaps, determine if the existing protocols are adequate and lay-out a roadmap to rectify. They also stress that they will seek involvement of consumer representatives and privacy advocates to insure their input is included early on in the process.
By February 2010, begin filling the gaps and modify protocols and standards where necessary.
Launch beta in early Q2’10 moving mock PHI over the Health Internet to test the system, make modifications and hardened the network.
Though they did not go so far as to say when the Health Internet will move live PHI, our estimate, assuming all goes relatively smoothly, is that the Health Internet will be open for business by late Q2-early Q3’10. This is a very fast track for the Health Internet, but certainly doable as the core infrastructure is already in place and this exercise is more of a fine tuning effort, than building from scratch.
Putting on the Pragmatist Hat:
Chilmark is very encouraged by the idea of the Health Internet and the new direction it is taking, creating a consumer directed and controlled interstate for the secure transfer of PHI. Not only does it finally acknowledge that at the end of the day, all the HIT spending in the world will make little difference if we do not get the one who has the most to gain, the consumer, involved, but this initiative may also create a fertile environment for innovation to occur.
But there are some challenges ahead for the Health Internet, which include:
The DURSA (Data Use & Reciprocal Support Agreement), which all NHIN (Health Internet) users (data providers, services, ISVs, etc) must sign to participate, stipulates that participants must abide by HIPAA requirements. Now HealthVault is on record stating that they have no problem with HIPAA, but Google is another story where they have been fairly adamant that HIPAA does not apply to them. Will Google now agree to HIPAA? And what about other ISVs and service providers, will they adhere to the requirements in the DURSA?
Beyond the feds and HIPAA requirements, there is a morass of state-specific laws as it pertains to the release of PHI, many of which go far beyond HIPAA in their requirements. As the Health Internet looks to create one common “health interstate” for the movement of PHI, how will these state laws be reconciled to allow this to occur?
Lastly, there is the issue of bringing awareness to the public. While the vast majority of consumers use Google for a second opinion, very few use the Internet to store, access and share their records. Very few even know what a PHR is. Whenever the topic is raised in conversations with lay people, maybe one person might have heard of Google Health or HealthVault, but it is a rare person indeed that has any understanding what these services are for and why they might be interested in using such a service. This may ultimately be one of the biggest challenges for Chopra and Park, but to their credit, they are making the right moves now, garnering industry backing who can assist them in “getting the message out.”
Chilmark Research will assist as best it can from its vantage point.
Aneesh and Todd, we are in!




John – good post.
The issue with State level provisions is a difficult one – but a few states have a fair amount of resources dedicated to helping with the gap analysis. Ex. – Florida Agency for Health Care Administration has a “Crosswalk Tool” http://www.fhin.net/
“Will Google now agree to HIPAA?”
Even without agreeing to HIPAA, my understanding of the Privacy & Security provisions in the HITECH Act is that it imposes similar penalities for Business Associates ( PHRs included), as HIPAA does for Covered Entities. As such, Google will still be subject to the privacy and security provisions in HITECH – even if their rhetoric remains anti-HIPAA. The real question still remains – as you posted a few weeks ago – “https://chilmarkresearch-v2.mystagingwebsite.com/2009/08/06/is-google-health-irrelevant/”
John, Thanks for the recap. Big step.
Your statement about RHIOs “in regions where competitors willingly chose not to compete on data, rather seeing value in sharing data” I think this will take a while. Many businesses/hospital/facility like their “walled garden” and see it as a way to retain patients/customers. Hospital provide “EMR Donations” program to capture and retain market share.
I am in total agreement with you on getting the consumer, involved is the most crucial key to success. It will take some type of incentive to make this happen. At the Hospital de Italiano in Buenos Aires, The doctors that I spoke with were surprised at at the usage of their PHR by elderly patients. The reason was that the patient could save more than 10 min by making an appointment on the PHR rather than the phone.
Jeff Brandt
http://www.motionPHR.com for the iPhone
Tom,
Didn’t Google have the problem with the “HIPAA Business Associate Agreement”. Microsoft make you sign one.
John,
Thank you for the post. I am linking it to “MedTech-IQ”, an international Wenb 2.0 community dedicated to the 3C’s of “Content, Community & Collaboration” in advanced medical technology, http://medtechiq.ning.com/. See post, http://medtechiq.ning.com/group/medicalinformatics/forum/topics/an-important-new-development.
CC
Jeff- my understanding of the provisions – PHR data handling, privacy & security will be governed by the provisions in the HITECH Act – even if Google does not want call itself HIPAA Business Associate. So in essence, HITECH reaffirmed HIPAA and put additonal measures in place to cover those entites that evaded HIPAA penalties. Again – thats my understanding – perhaps there are a few experts reading this post who can clarify further.
John: Great post, and exciting news for those of us in the PHR community who have been doing pick and shovel work for quite some time. That missionary work is finally paying dividends, and signs ranging from patient engagement requirements as part of meaningful use criteria to this NHIN news indicate that recognition of PHR (or PHP) value is growing.
Our experience also shows that with the right targeting, PHRs are embraced and adopted. This year, 40% of the incoming freshman class at Indiana University’s main campus created an IU branded PHR prior to arriving on campus. Better yet, half of those students have used the PHR since school began to interact with the student health center. Last week, IU integrated its online appointment scheduling app with the PHR and registrations spiked again. Combine tech-savvy students who insist on conducting business online with helicopter parents who want to ensure the safety of their children, and you have a recipe for adoption and use.
Finally, having participated in the NHIN demo late last year, we have seen firsthand the power of connecting a PHR with the NHIN. It opened our eyes to the power of the Health Internet concept.
John, great post! One thing I heard differently — Todd is pushing for REAL patient data in Q2 2010, not fake information — which makes it extra-awesome from our perspective.
Here at HealthVault we are marshalling our team to help make it happen — feels like it could be a real tipping point.
The exciting part about this new approach is getting more industry “outsiders” (e.g. MS & Google–soon to be insiders) involved. The healthcare industry has existed as a “closed universe” for too long. These technology organizations have experience in building standards and API’s that work, even if they are not blessed as the one single enabling approach.
We are not going to have a “single enabling approach” anytime soon, interoperability will grow organically just as it has on the Internet. We need stakeholders to cooperate and innovate at the same time. The “Health Internet” is going to be a fluid, evolving, infrastructure for some time to come. This is as it should be!
John,
Great post.
You write: “But what might happen if the folks in DC stopped talking about the NHIN as some uber-Health Exchange, but instead positioned it as a consumer-focused platform?”
Do you really mean “instead”? or “in addition to”?
Are we just reconceptualizing NHIN as not only B2B, but B2C and C2C?
Great Post!
How many understand that if there are not fundamental process changes in how the data originating from patients and the physicians they trust is created, all the fancy, top-down solutions promise to be little more than a lot of expensive technotitillation?
How many in the industry and government are still mostly focused on technotitillation rather than creating the the necessary bricks that are the foundation? Who has realized that physicians are not great brick-makers or data-entry clerks?
Who has a clue that absent the data from the patient-physician interface, none of the rest of it matters very much?
I think the NHIN, as it is today, is already dated architecture. No one is talking about its scalability, privacy and security.
I think Chopra and Park have it right… a Fed centric network won’t work, won’t be robust enough and will never…ever reach the consumers. And there’s lots of legal hurdles that will have to be overcome.
I think they should scrap the most of the NHIN/CONNECT and work at the state and local levels to set up the backbone. The Feds already have a National Information Exchange Model (NIEM) that’s in use today across several large federal agencies. Why do they need a second one vis e’ vie, the NHIN?
You’re talking tens of years before we’ll have substantial EMR penetration and even longer for PHRs. It will take many more carrots and many more sticks to drive this.
Therefore, I believe we’ll see a clearinghouse/brokerage model for clinical information emerge even more strongly in the next 5 years.
That’ll be the avenue to get the consumer in the value chain faster.
It’s about time. Consumer engagement is one of the most essential ingredients to the healthcare transformation and for the past 4 years, it has been left out of the equation.
Most of the HIE’s around the country, don’t really know how to evolve their current technology. The technology to this point, should really be scrapped. Google, Microsoft, and Health Banks get what they need so why not leverage what is underway? Why do we have to take what NHIN created and salvage it? Let’s admit that the first 4 yrs were a trial and admit that it won’t work and learn from others what will work.
I really hope that our money will go into finding out the right balance for the consumer and how to engage people in their own healthcare. After all, we have to change the habits of individuals if we want to make a dent on our spending. While clinicians may not like the change they must also endure to improve quality and reduce cost, we do understand that clinician change is needed. With meaningful use incentives will be aligned.
Now if we can get incentives to be provided by insurance companies, employers, and the states to help individuals become engaged, we will make progress.
John:
Great post!!
As an active member of the Health Record Bank Alliance (HRBA), an organization promoting the consumer as the true owner of their personal health information with complete access to and ultimate control over its disposition, it is refreshing to see this important shift in strategy. To borrow your highway analogy, spending billions of dollars to motivate provider adoption of EHRs is like putting a sleek car in the garage with no roads built to drive to the highway…..pretty to look at…..but not very useful if you can’t connect to anything “meaningful.”
To date, as everyone well knows, consumer engagement, while referenced frequently across most of the health information technology venues, is pure lip service, marginalized in the greater effort to implore healthcare stakeholders to play in the same sandbox together.
Adoption of the Health Record Bank model solves the problem of withholding data by competing interests. If the consumer asks for their data, by law, it must be released to them…..done deal!
I am sure that Bill Yasnoff, MD, Executive Director of the HRBA would be interested in sharing his views on this topic. I wanted to share the HRBA website with everyone and point to the HRBA Principles document linked on the home page:
http://www.healthbanking.org/index.html
There is a long way to go, but it’s a start……….we are “ALL IN.”
RFV